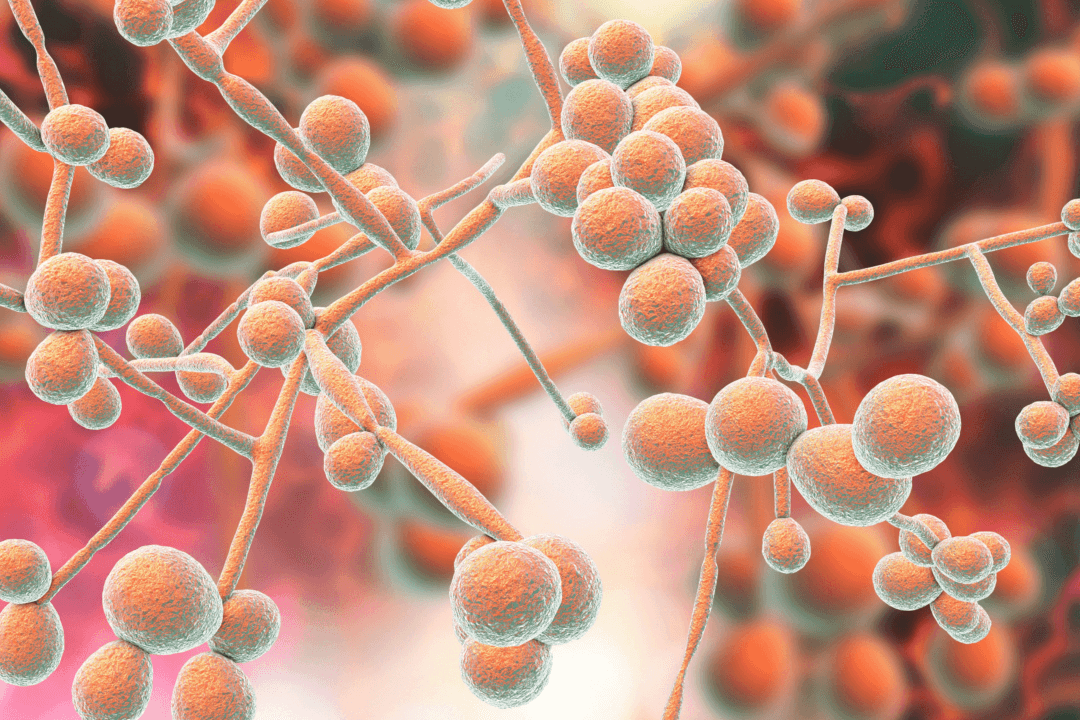
Most people think of a fungal infection as something like a yeast infection or athlete’s foot—they’re itchy and annoying but harmless and relatively easy to treat. However, there are various species of fungi lurking around the world, preying on people with weakened immune systems. Once these fungi enter the human body, they can resist standard antifungal drugs and often cause serious illness or death.
One type of fungus that’s been getting recent media attention, Candida auris, is becoming more prevalent throughout the United States and the world, with a steadily rising death toll. It’s difficult to detect through blood tests because it looks like other, more easily treatable fungal infections. Once it’s identified, treatment can be challenging because of inappropriate management from prior misidentification and the infection’s ability to evade and resist current drug treatments.