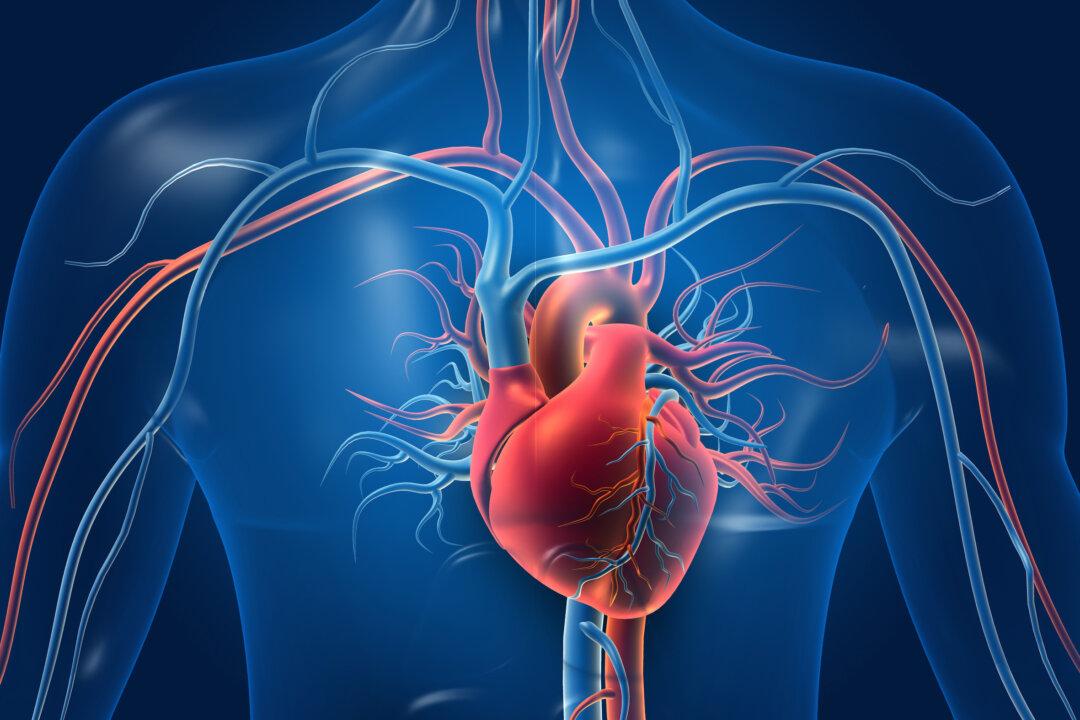
Scientists from Melbourne University have engineered a fast and scalable approach to making blood vessels using natural tissues.
The research team applied a novel approach to tissue engineering of blood vessels led by Redmond Barry Distinguished Professor Andrea O’Connor and Associate Professor Daniel Heath, both of whom are from the Department of Biomedical Engineering at Melbourne University, Australia.