Almost one in five people (19 percent) have witnessed or received “corridor care” in NHS hospitals in the last six months, according to a YouGov poll commissioned by the Royal College of Nursing (RCN).
RCN General Secretary and Chief Executive Professor Nicola Ranger said: “The public and nursing staff can see a tragedy for patients unfolding before their eyes. They know care standards are unacceptable and they want government to act decisively.
“The first step it can take to protect patients from corridor care is to introduce mandatory reporting of any time it takes place.”
Responding to the poll, a Department of Health and Social Care spokesperson told reporters that it was “shocking that corridor care has become a feature of the broken NHS this government inherited, but we are determined to change this.”
The spokesperson said the government was investing £26 billion into the NHS and social care over the two years.
Patients Dying in Corridors
The poll was conducted after the RCN released its Jan. 16 report into corridor care, which detailed the experiences of nurses trying to care for patients outside of designated treatment areas.The report, which recounts the experience of more than 5,000 nursing staff across the UK, including 4,000 from England, who said they had cared for patients in corridors, storerooms, carparks, offices, and toilets, with some patients, including the elderly, sitting in chairs “for days.”
They also detailed how they had faced situations where they were trying to treat people without having access to critical facilities like oxygen, suction, or monitoring equipment.
One nurse told the report authors that a patient died in the corridor “but wasn’t discovered for hours.”
“I had to change an incontinent, frail patient with dementia on the corridor, by the vending machine. It was undignifying,” said one nurse.
“Department was overwhelmed, which is a daily occurrence. Flow has to be maintained despite space/staff limitations. At its worse asking someone to go round and make sure people are still alive,” detailed another.
Several others quoted throughout the report had described the situation as being similar to a “third world” country or war zone.
No Longer a Winter Problem
Following the RCN’s January 2025 report, the Royal College of Physicians (RCP) issued its own statement, calling on the government to take immediate action to end corridor care.The RCP said that crowding in emergency departments had become increasingly prevalent in the last several years, but had escalated in the past 12 to 18 months.
The professional membership body said in December 2024 alone, over 54,000 patients in England waited over 12 hours in accident and emergency rooms for admission, with many likely receiving care in inappropriate locations.
RCP Clinical Vice President Dr. John Dean said he welcomed NHS England’s plans to start recording data on instances of corridor care, but added that “this data must be clearly defined, published as soon as possible, and reported regularly all year round.”
“‘Corridor care’ is no longer a problem confined to the winder months,” Dean said.

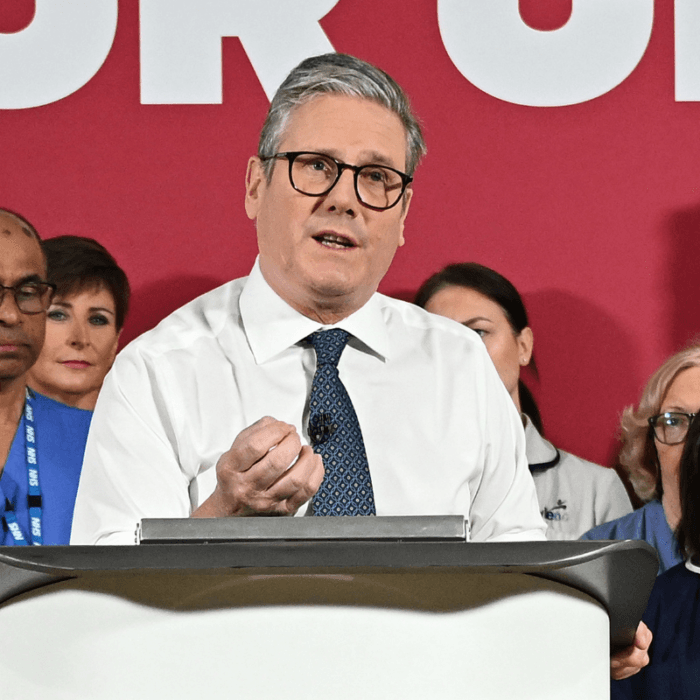
Streeting told the House of Commons, “It is unsafe, undignified, and a cruel consequence of 14 years of failure on the NHS, and I am determined to consign it to the history books.”
However, the minister admitted that he could not promise that patients will not be treated in corridors next year.
“It will take time to undo the damage that has been done to our NHS, but that is this government’s ambition,” he said.