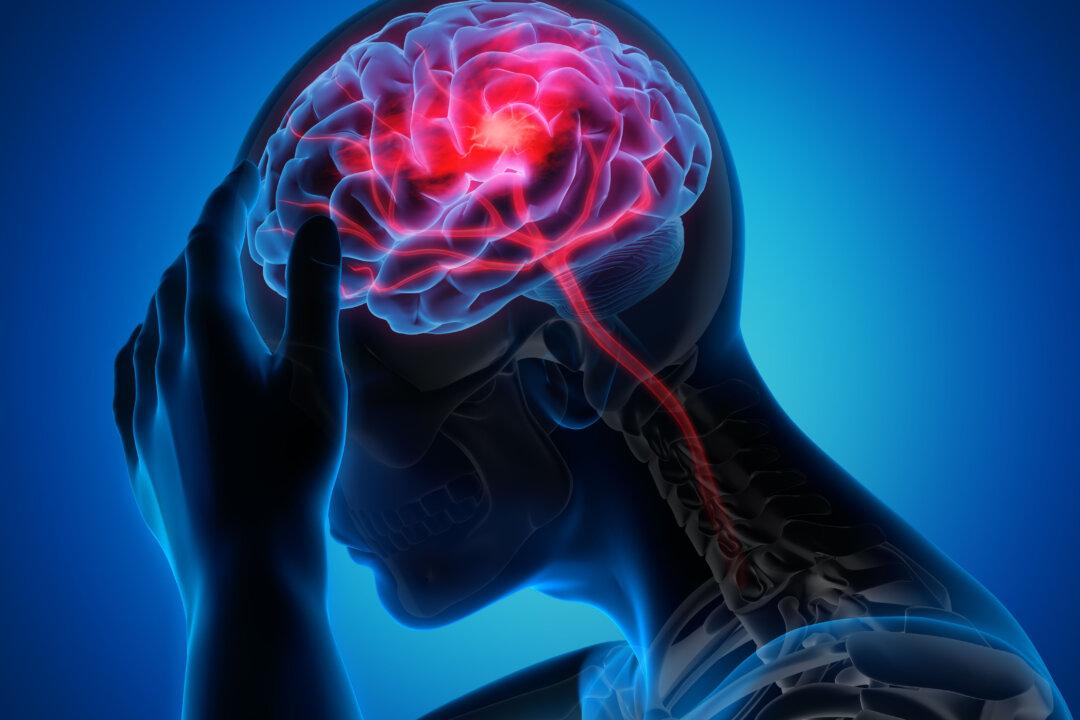
Someone is diagnosed with the condition every four seconds. New research finds common virus infections are linked to developing a degenerative brain disease. But experts also have different opinions.
Common Virus Infections Associated with Neurological Disease Risk: Study
“We are seeing mounting evidence,” Heather Snyder, Alzheimer’s Association vice president of medical and scientific relations and who holds a doctorate in molecular biology, told The Epoch Times, “that microbes and/or viruses in the brain may be triggering or contributing to some type of immune reaction” that is related to the buildup of amyloid plaques and tau tangles—the hallmark of Alzheimer’s disease.This is not limited to Alzheimer’s disease. Researchers at the National Institutes of Health (NIH) found an association between exposure to various viral diseases and an increased risk of many neurodegenerative diseases.