Commentary
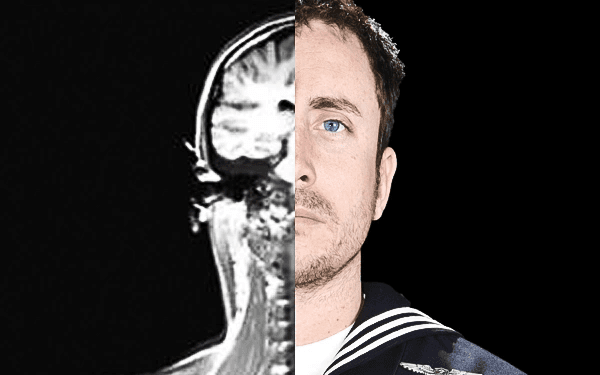
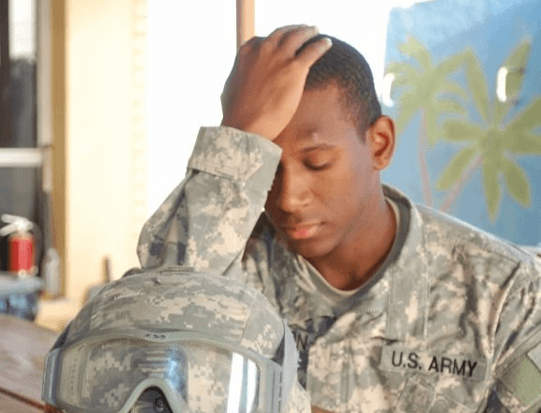
It has been known for over 80 years that following a head injury there is dysfunction in the hypothalamic-pituitary-adrenal (HPA) axis. According to the Centers for Disease Control (CDC), 80–85 percent of traumatic brain injury (TBI) sufferers are classified as mild traumatic brain injuries (MTBI). Approximately 80–85 percent of MTBI patients recover from their injuries, while approximately 15–20 percent continue to experience persistent symptoms. Fifty percent of those TBI patients end up with some type of hormonal imbalance in the HPA axis. This brain injury-related condition is commonly referred to as neuroendocrine dysfunction (NED).