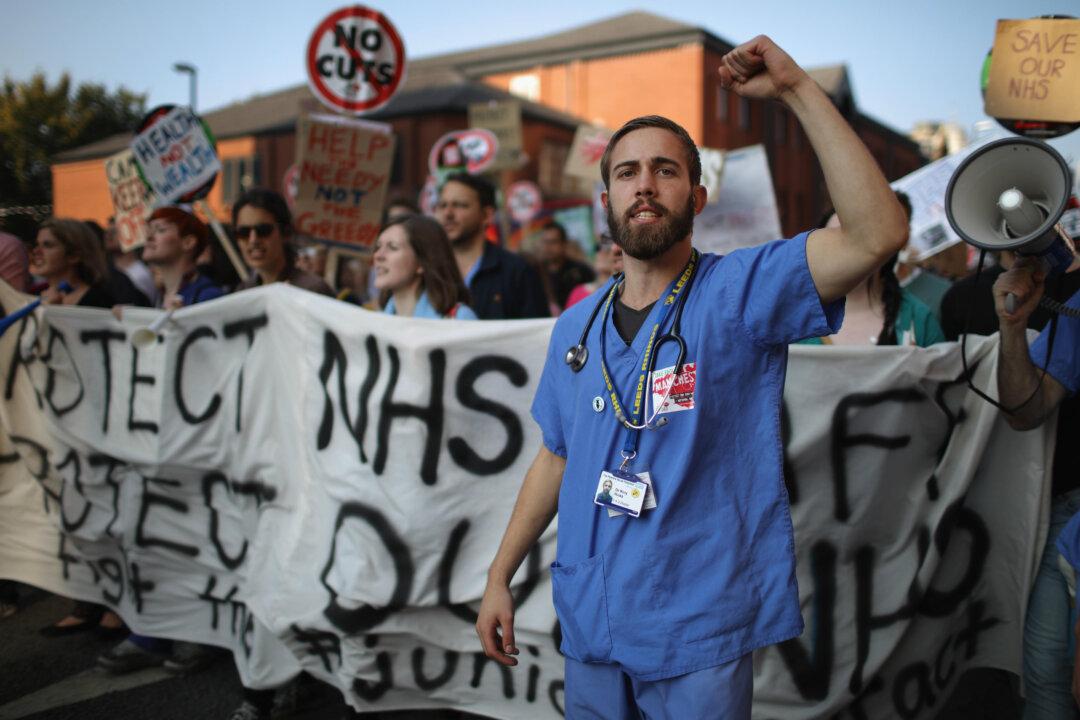
The current threat of a doctors’ strike is just the latest example of the unhappiness of U.K. National Health Service (NHS) staff. In 2014 we saw strikes from nurses, occupational therapists, porters, paramedics, and health care assistants—the first in the health service since the 1980s. Staff is being asked to make huge efficiency savings after years of small or nonexistent pay increases. Morale has plummeted as health care workers come under fire for the quality of NHS care.
The latest conflict is over the planned introduction of a full seven-day service. Junior doctors are being asked to accept a cut in overtime pay in return for an increase in basic pay so that it becomes cheaper for hospitals to employ more staff on evenings and weekends. In response, the doctors have threatened to strike, while the number of physicians applying for documentation to work abroad has soared.