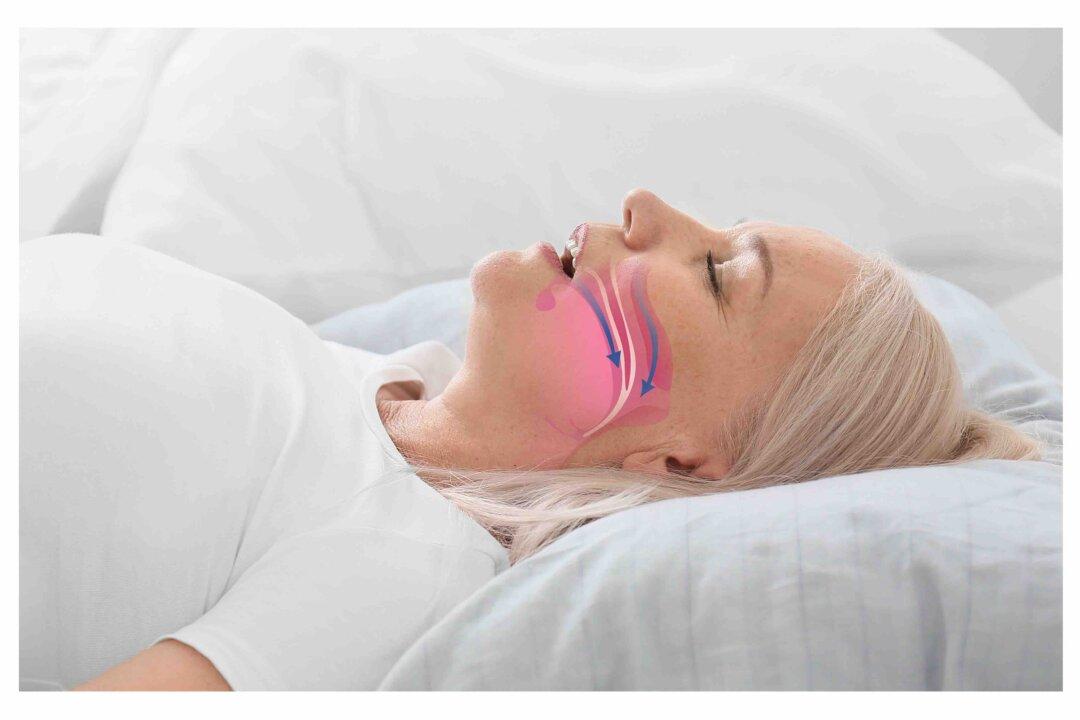
Over the past couple of years, with the pandemic and its shutdowns, work schedule interference, and indeed job loss, etc., many people naturally have developed greater levels of stress and anxiety.
Functionally, this often shows up as clenching the teeth during the day or night. The teeth are unconsciously pressed together with maximum biting force. When we eat, there is something in-between the teeth—food—which means that most often the teeth do not fully come together; but in clenching, it is full tooth-to-tooth contact.