The parents of two children who died after the NHS went to court to withdraw their treatment are locked in a Supreme Court battle with the hospitals for the right to name the doctors involved in their treatment.
Two NHS hospital trusts are appealing a High Court decision last year that granted the families of Zainab Abbasi and Isaiah Haastrup the right to name the doctors involved in the decision to withdraw life support for the two very sick children.
The court ruled last March that the risk to privacy for the hospital staff was outweighed by the parents’ rights to freedom of speech in being able to tell their story.
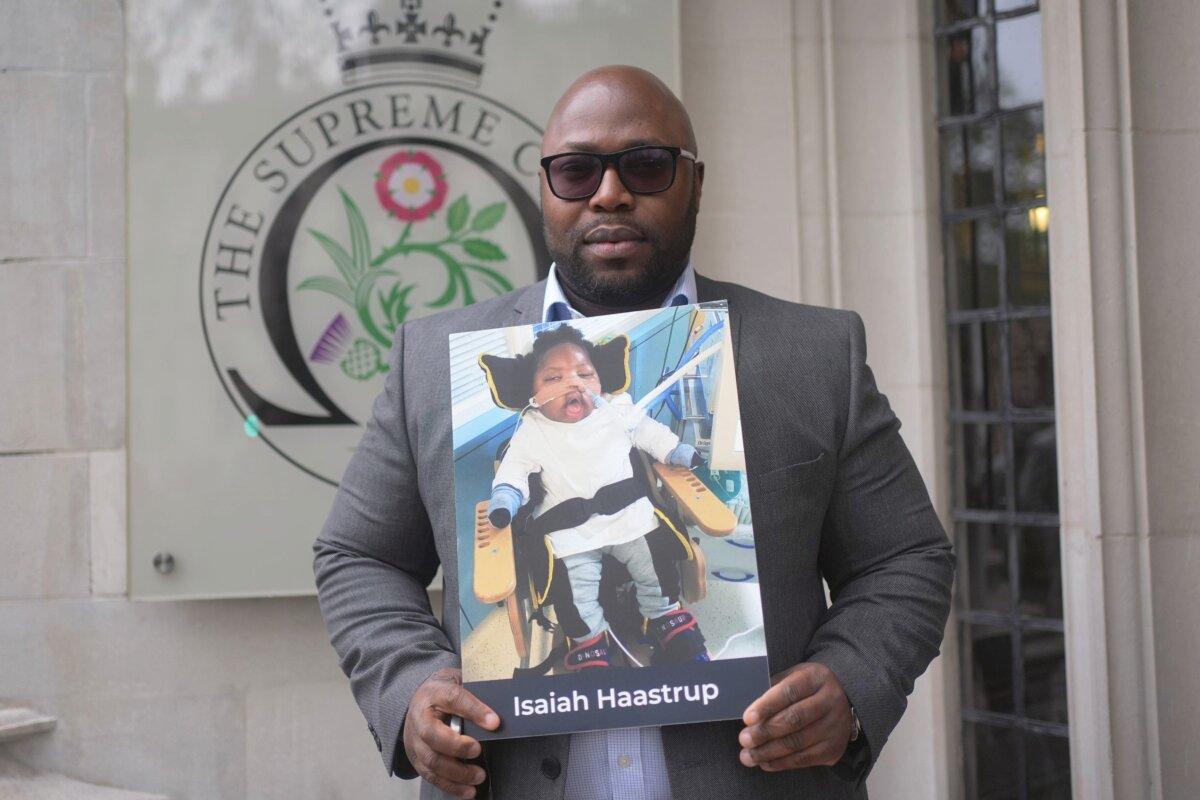
Isaiah was left severely brain damaged after he was starved of oxygen at birth. A judge ruled that it was not in his best interests to keep him on life support, but his parents, Takesha Thomas and Lanre Haastrup, both opposed allowing him to die and fought the decision. He died aged 12 months in Kings College Hospital, London.
Zainab suffered from a rare genetic illness—not diagnosed until she was three—and was being kept alive by a ventilator that doctors at Great Northern Children’s Hospital in Newcastle wanted to remove when she was 6, saying it was not in her best interests to prolong her life.
Her parents, both doctors themselves, virulently opposed withdrawal of treatment and had to be dragged away from their daughter’s bedside by police officers, who arrested her father Rashid. He was de-arrested after he suffered a heart attack.
Following the incident, the NHS trust applied to the High Court for permission to take Zainab off the ventilator, but she died in September 2019, three days before the hearing was due to start.
The Abbasis told media at the time that police officers were “being barbaric” towards them, and described the situation as like “living a nightmare.”
In the case of both children, indefinite Reporting Restriction Orders (RROs) were initially granted, prohibiting the naming of medical professionals involved in their care and the decision to withdraw it.
Both sets of parents appealed against the orders made in the Family Division of the courts allowing the continuation of the RROs, on the basis that they prevented the families from having meaningful public discussion about the circumstances in which their children were treated and died.
It is also claimed that the restrictions prevent the media from being able to accurately report on or discuss the cases.
In Zainab’s case, the RRO prohibits the naming of the small cohort of medical professionals directly involved in her care. In Isaiah’s case, the range of medical staff protected is wider.
The Court of Appeal last year found in favour of the families and discharged the restrictions, but the order was stayed pending an appeal to the Supreme Court made by the two hospital trusts, Kings College Hospital Trust and Newcastle-Upon-Tyne Hospital NHS Foundation Trust.
‘Medical Gaslighting’
After the High Court granted the lifting of reporting restrictions last year, the Abbasis said: “Our family has suffered so much due to the actions of the hospital. As doctors ourselves we were aware of the medical gaslighting and the appalling mistreatment our daughter was subjected to but we were rendered powerless to take effective action by the injunctions the hospital obtained which served only to protect a toxic culture which puts doctors’ interests before those of their patients.”“The transparency which the Court of Appeal has endorsed will ensure proper accountability within the medical profession and help restore ethical standards and public trust in the NHS.”
The couple claimed they have been gagged from revealing the “inappropriate attitude” of clinicians, the “lies” told by some medics giving evidence, and details of how a senior doctor refused to meet with consultants employed by the family.
Isaiah died after a judge gave permission to medics to provide only palliative care. Specialists told Mr. Justice MacDonald that providing further intensive care treatment was futile and not in his best interests.
Hospital bosses admitted liability for “events surrounding the birth” of Isaiah and settled “an action for medical negligence” brought by Mr. Haastrup in 2021.
Ahead of Monday’s Supreme Court hearing, Mr. Haastrup said, “I want to tell my story, my story is not complete when the characters are not named.”
Mr. Haastrup said he could understand “at that time” why the reporting restriction was made but said it was now “academic.”
“There’s no point of having it in place any more,” he said, adding that his son had been a “fighter.”

Mr. Haastrup has claimed that the original gagging order prevented him from revealing details of medical negligence during his son’s birth, of the “financial motivation for taking the end of life route,” and the details of his death.
Gavin Millar, KC, acting for the two NHS trusts, said that the Court of Appeal’s decision to allow the naming of staff “contains a number of clear and obvious missteps.”
In written submissions for Monday’s hearing, the barrister said the judge who originally upheld the court orders “had well in mind the fact that the identities of the clinicians would be publicised in conjunction with allegations being made against them by the parents, connected to the emotive issues in the end-of-life proceedings.”
Alex Ruck Keene, KC, for the Faculty of Intensive Care Medicine, said in written submissions that some health care professionals in high-profile end-of-life cases have faced “intimidating behaviour and death threats” as well as being “named and shamed” on social media.
‘Justice for the Families’
Several families, including the parents of Indi Gregory and the mother of Archie Battersbee who were also involved in high-profile court cases over their treatment prior to their deaths, attended the Supreme Court on Monday to support the parents of Zainab and Isaiah.Indi’s father Dean Gregory said, “We just want justice for the families who are going through what we’ve been through and to be able to tell the story because the professional doctors have nothing to hide.”
He added: “We don’t want anyone going through what we’ve been through … It felt like as parents we had no rights, Indi had her rights taken away.”
The family of 19-year-old Sudiksha Thirumalesh, who had a rare mitochondrial disorder, also attended the start of the two-day hearing in central London.
She and her family could not be named until after her death last September, with the NHS trust and doctors identified later.
Her brother Varshan Thirumalesh said: “Emotionally it felt like we were being jailed. We are here to tell her story to the whole world. She has been gagged for a very long time.
“It shouldn’t happen to any other family after this.”

The hearing before five Supreme Court judges will consider evidence from a number of medical bodies, including the British Medical Association and the Royal College of Nursing.
The families are supported by Christian Concern and the Free Speech Union, and the ruling could have widespread ramifications for reporting of the family courts.
The hearing is set to conclude on Tuesday, with a judgment to be handed down at a later date.







