The survey of 283 practices found that 46 percent were already taking some kind of action while a further 20 percent said they were planning to do so. Just 7 percent of practices ruled out taking any action.
Earlier this month, family doctors in England voted overwhelmingly in favour of industrial action after their union took a ballot.
BMA Ballot
According to the British Medical Association (BMA), more than 8,500 GPs cast a vote, with 98.3 percent backing collective action.The BMA has issued a list of 10 non-contractual actions for surgeries to choose from, including GPs limiting the number of patients they see each day to 25.
Other proposed actions include choosing not to perform work they are not formally contracted to do, (known as “working to rule,”) refusing to share patient data unless it is in the best interest of the patient, and referring patients directly to specialists rather than following the usual NHS processes.
Practices could also potentially ignore “rationing” restrictions on medications by “prescribing whatever is in the patient’s best interest.”
More than a quarter of the practices that responded to the Pulse poll were limiting the number of patients who could be seen each day by a GP while 44 percent said they were considering it.
Last GP Strike was 60 Years Ago
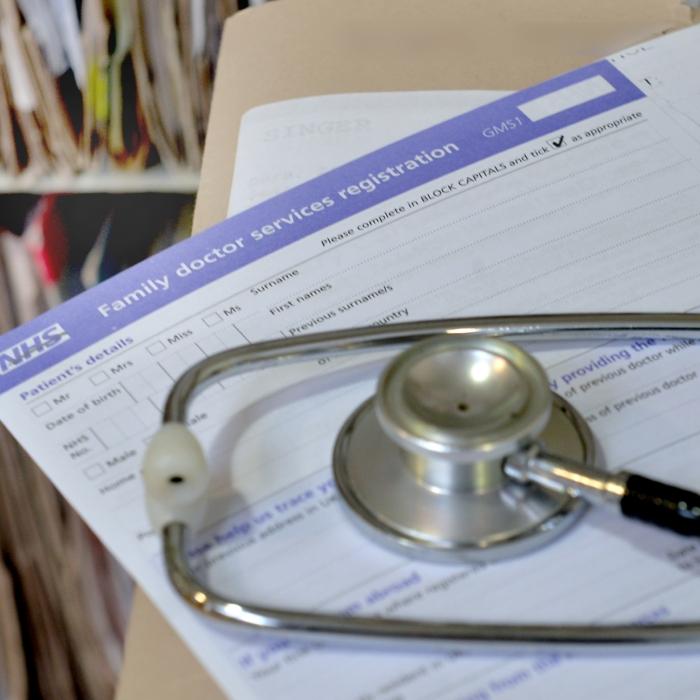
GPs have not gone on strike in the UK since 1964, when family doctors collectively handed in undated resignations to Harold Wilson’s Labour government. This action led to widespread reforms and the creation of a Family Doctor Charter in 1965.The BMA is calling for a new Family Doctor Charter to be signed by 2025, which they say should commit to increasing spending to 15 percent of the NHS budget on general practice to make it “the jewel in crown” of state healthcare provision.
Dr. Amanda Doyle, NHS director for primary care and community services, said: “We will be monitoring the impacts of this action to ensure practices fulfil their contractual requirements and continue to meet the needs of patients.
‘The Front Door’ to the NHS
Dr. Michael Mulholland, said on behalf of the Royal College of GPs (RCGP) said that the current GPs contract was “failing” to provide the necessary support for surgeries.“General practice is the front door of the NHS, but it has faced years of underfunding and neglect, and is now seriously struggling.
“It is not for the RCGP to get involved with contract negotiations between the BMA and NHS England, nor to influence how practices participate in collective action.
“No GP will want to restrict the services they provide for their patients, so we hope that the Government is able to intervene to help reach a fair resolution as soon as possible, so GPs have the funding and support to provide the care our patients need.”
A Department of Health and Social Care spokesperson said: “This Government is committed to shifting the focus of healthcare out of hospitals and into the community, to fix the front door to the NHS.
“We have already accepted the independent pay review body recommendation of a 6 percent uplift in GP pay and committed to hiring an extra 1,000 GPs into the NHS by cutting red tape, through an £82 million boost to the additional roles reimbursement scheme.
“Collective action will only punish patients. NHS England has preparations in place to ensure patient safety is protected and patients should still come forward for care as usual.”