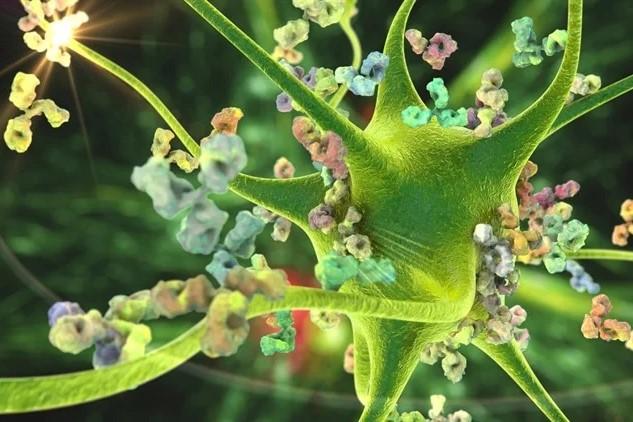
COVID-19 is accelerating the accumulation of senescent or “zombie” cells in the brain, which accumulate naturally and gradually in the brain with ageing, according to a new study from the University of Queensland.
The researchers used brain organoids—mini brains artificially grown from human stem cells—to study this effect.