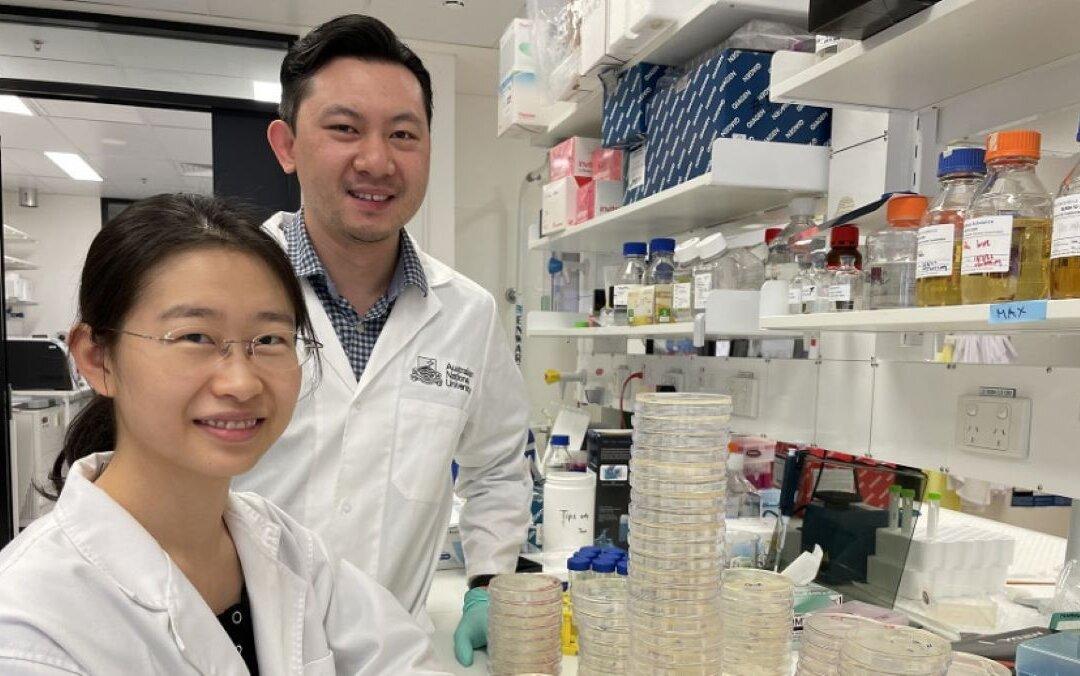
Australian researchers have discovered a specific group of bacteria-killing proteins innate to our immune systems, which may lead to the development of more effective drugs capable of combatting infectious diseases such as pneumonia, meningitis, and sepsis.
The Australian National University (ANU) team, which saw its findings published in Nature Communications, demonstrated the ability of these immune proteins to directly bind and destroy certain types of bacteria.