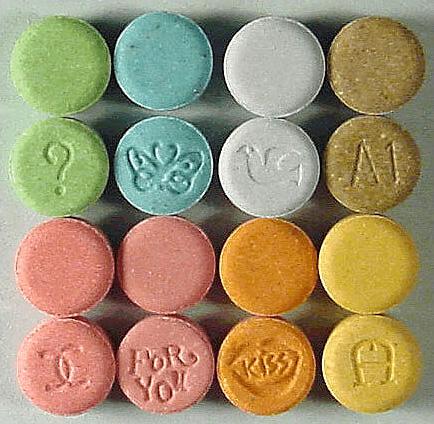
Australia will become the first country to reclassify medicines containing methylenedioxymethamphetamine, more commonly known as MDMA (ecstasy) and psilocybin, to treat certain mental health conditions.
The Therapeutic Goods Administration (TGA) announced on Feb. 3 that they will permit authorised psychiatrists to prescribe MDMA for Post Traumatic Stress Disorder (PTSD) and psilocybin for treatment-resistant depression.