With some countries rolling out their 5th booster shot against COVID-19, many are putting the necessity of the next dose in question. For some, the extra shots are recommended by the CDC, but this does not mean we should all jump on the vaccine wagon.
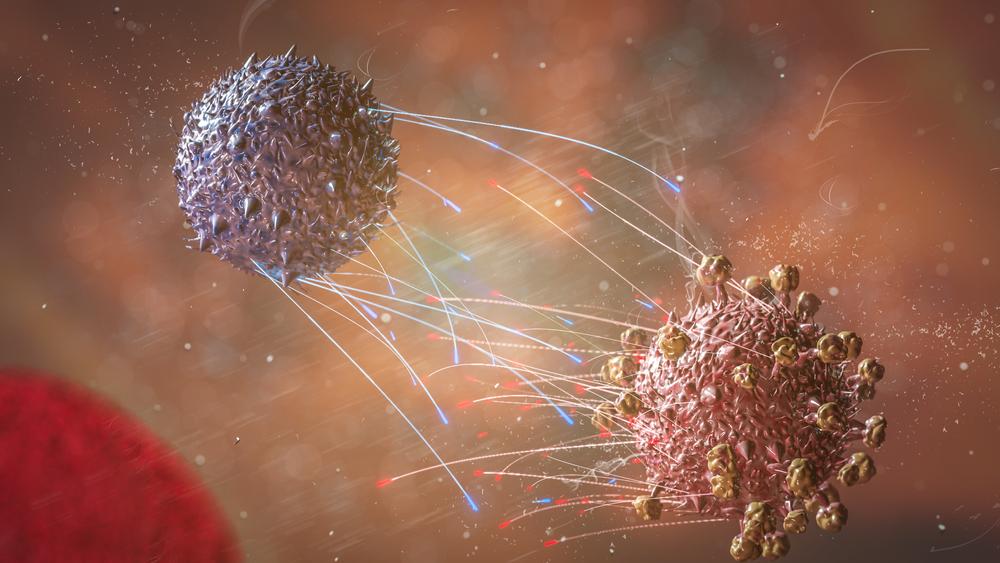
Given that almost 1 in every 3.5 Americans have already had a confirmed COVID-19 infection and that our natural immunity is said to be more resilient than a booster shot, there are more ways to bolster your own antiviral immunity.