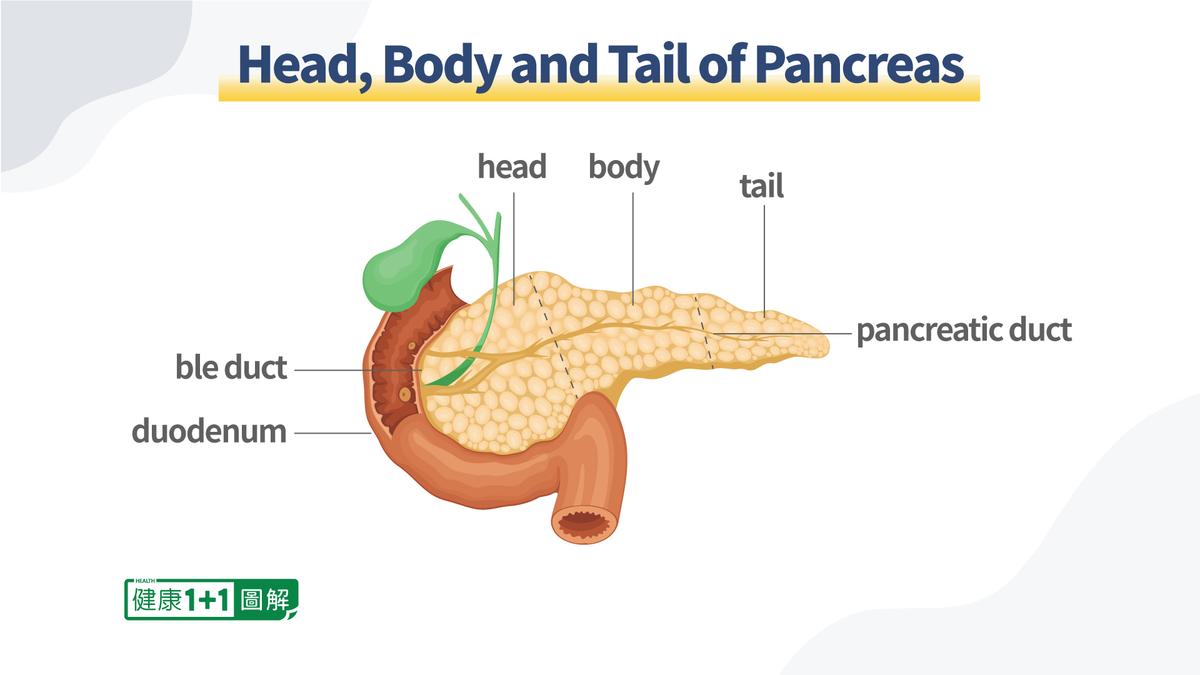
Located in the back of our abdomen, the pancreas is a long flattened organ and gland that is part of both our digestive and endocrine systems. The two main functions pancreas has are producing enzymes to help with digestion and sending the hormone insulin (among others) to control the blood glucose level in the body.