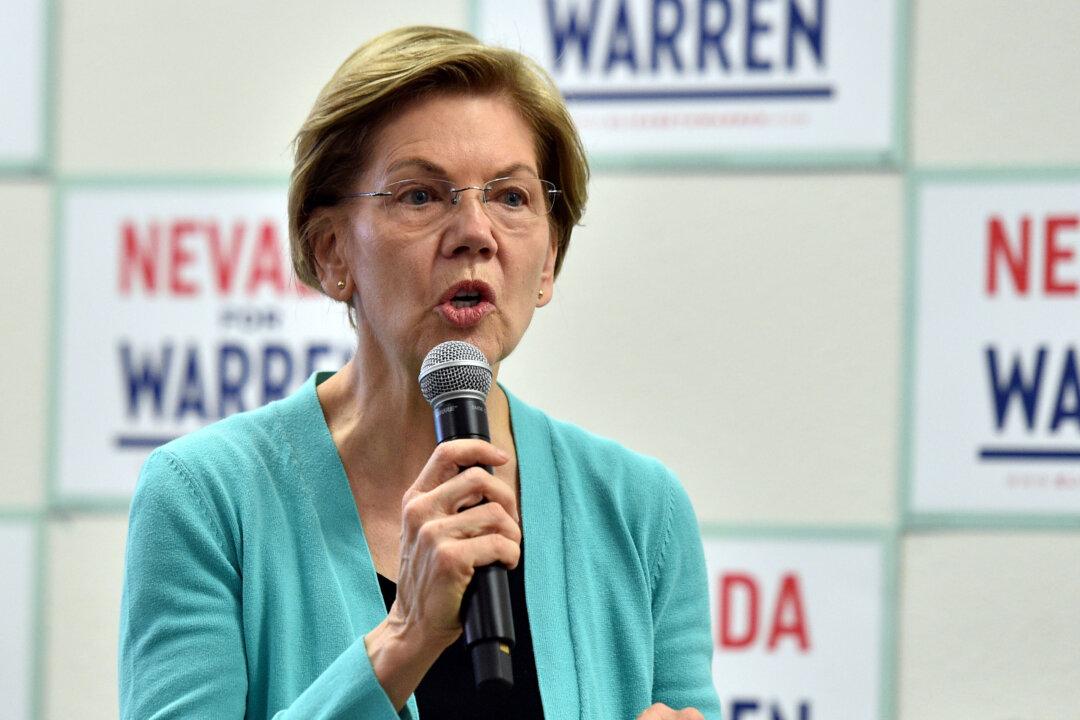
WASHINGTON—When Sen. Elizabeth Warren (D-Mass.) promised to “bring in 135 million people into Medicare for All at no cost to them” within 100 days of being inaugurated as president, she was just one of her party’s multiple White House aspirants touting dramatic expansion plans for America’s 55-year-old federal health care program.
Warren’s proposal, like that of her campaign rival Sen. Bernie Sanders (I-Vt.), would require a total reorganization of America’s $3.6 trillion health care system. It would guarantee comprehensive, government-funded and -managed health care, while eliminating private health insurance programs.