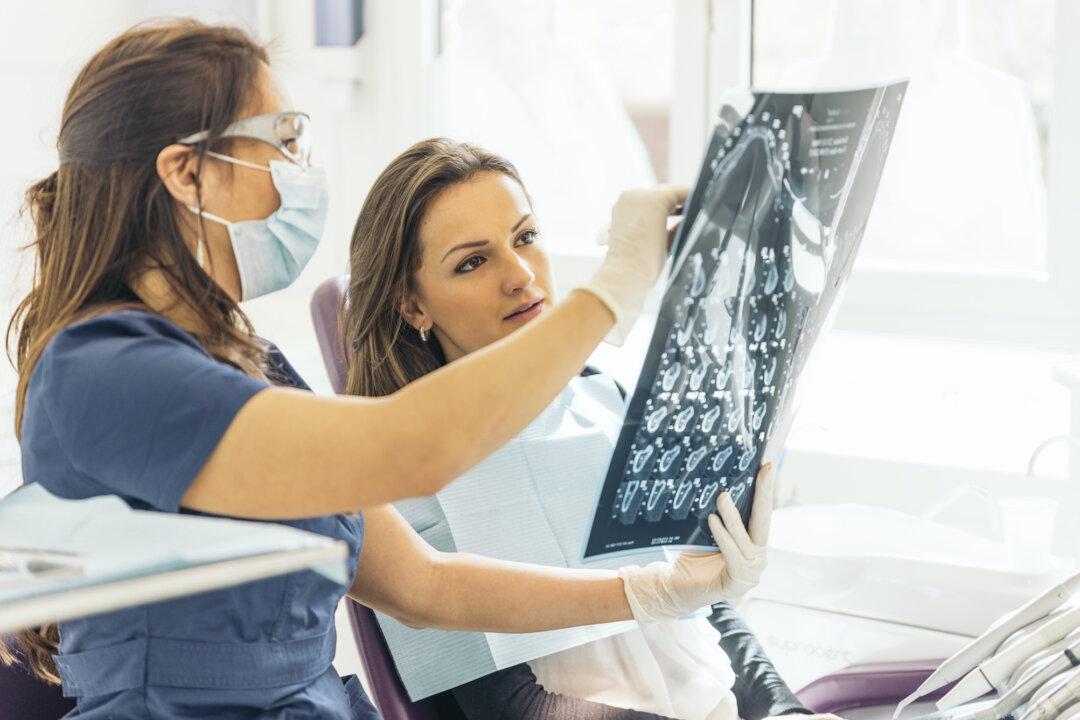
Untreated dental caries is the most prevalent condition worldwide, affecting 2.4 billion people and 32 percent of the population.
Why? It’s because we just love those sweet, sticky eats and drinks. It would not be so bad if we immediately rinsed with water to help neutralize the resulting acids, but of course we never do that as we like the taste.