Commentary
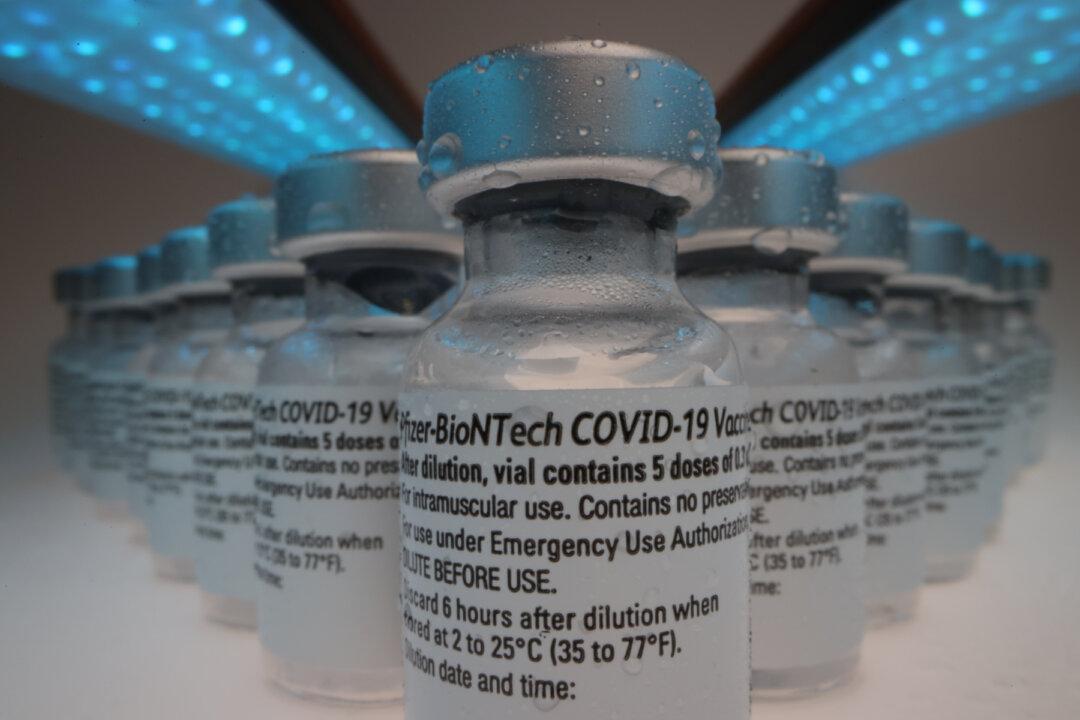
At the time of FDA approval for any vaccine, it is impossible to know whether it causes rare, unexpected serious adverse reactions. More than a year after the Covid vaccine approvals, we should have that information, but we do not. This is a serious problem.