Commentary
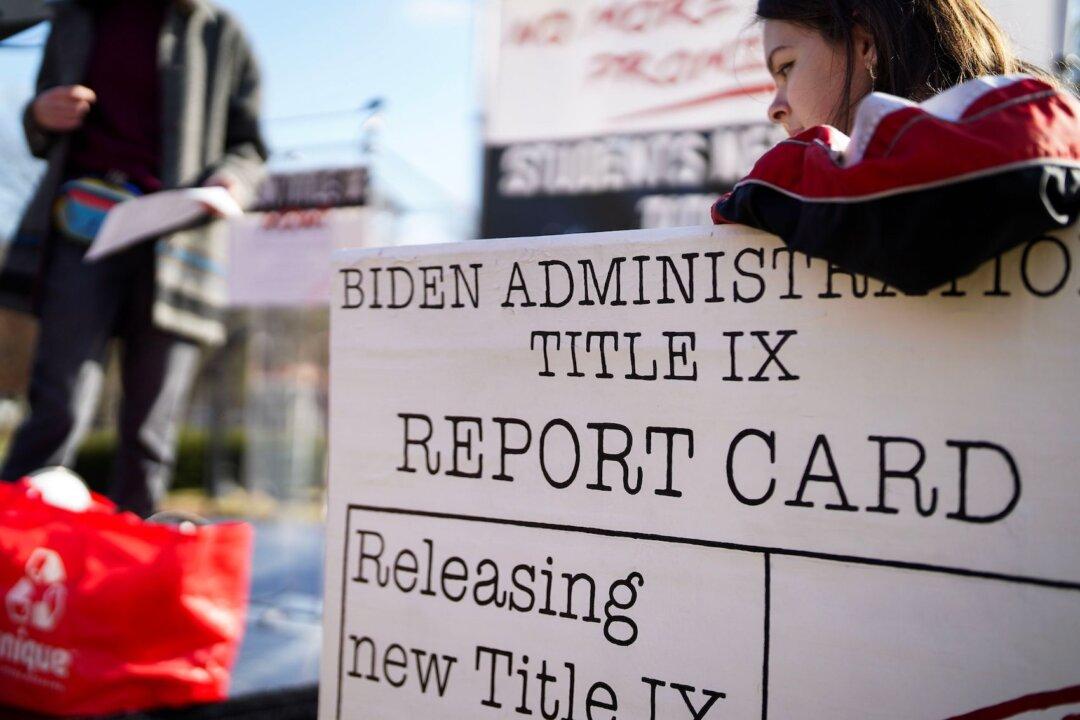
Last April, the influential New England Journal of Medicine published an advocacy column by a medical school professor that argued, “To promote equity, the Biden administration should distribute resources differentially in order to benefit groups that are persistently disadvantaged.”