Since the COVID-19 pandemic broke out, through mutations, the virus has generated many variants. The world has gone through many ups and downs as we respond to the pandemic in many ways.
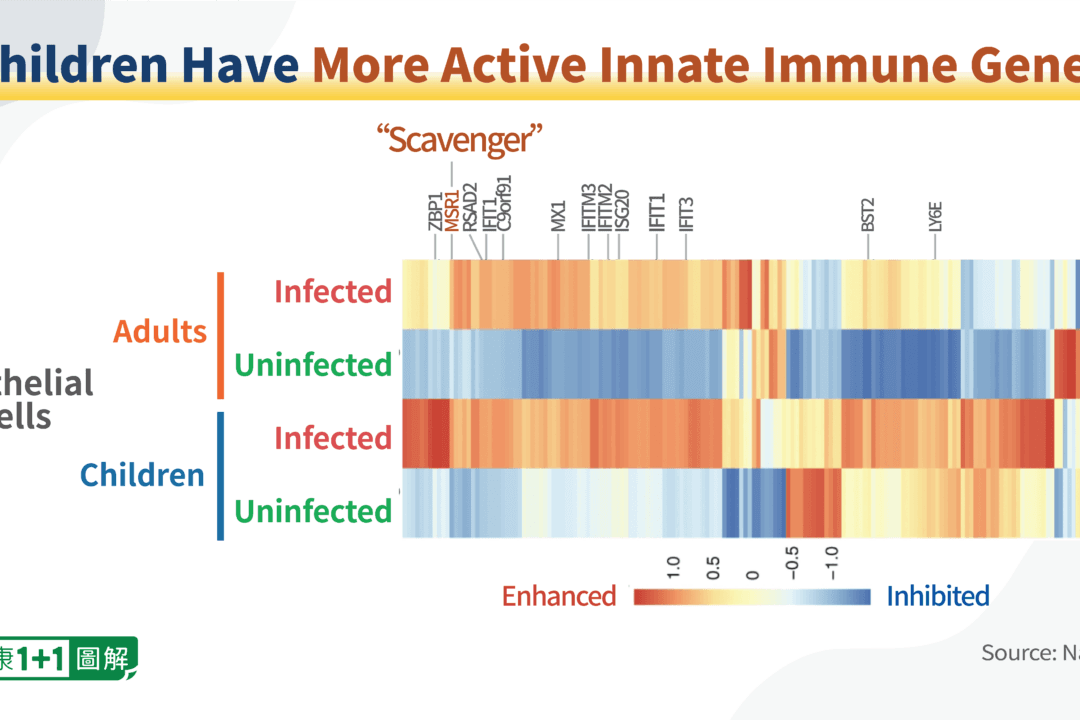
However, there is one group of people who have always been at the right end of the immunity spectrum: the children.