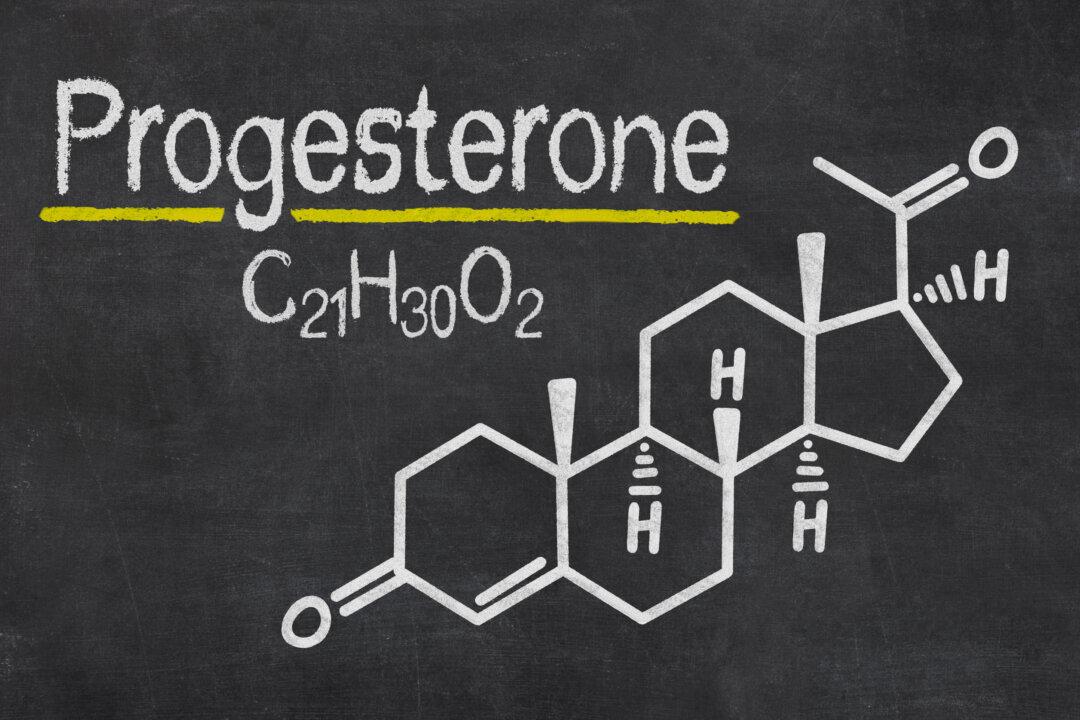
When a woman is pregnant, she is truly eating for two. Every food, medication, supplement and drug affects her growing baby. Her body also produces different levels of hormones to support the pregnancy. Each month, a woman’s body cycles through a variety of hormones that regulate the buildup of blood in the uterus to support a pregnancy, the maturation of an egg and the withdrawal of hormones that lead to menstruation.1
Dr. Joseph Mercola is the founder of Mercola.com. An osteopathic physician, best-selling author, and recipient of multiple awards in the field of natural health, his primary vision is to change the modern health paradigm by providing people with a valuable resource to help them take control of their health.
Author’s Selected Articles