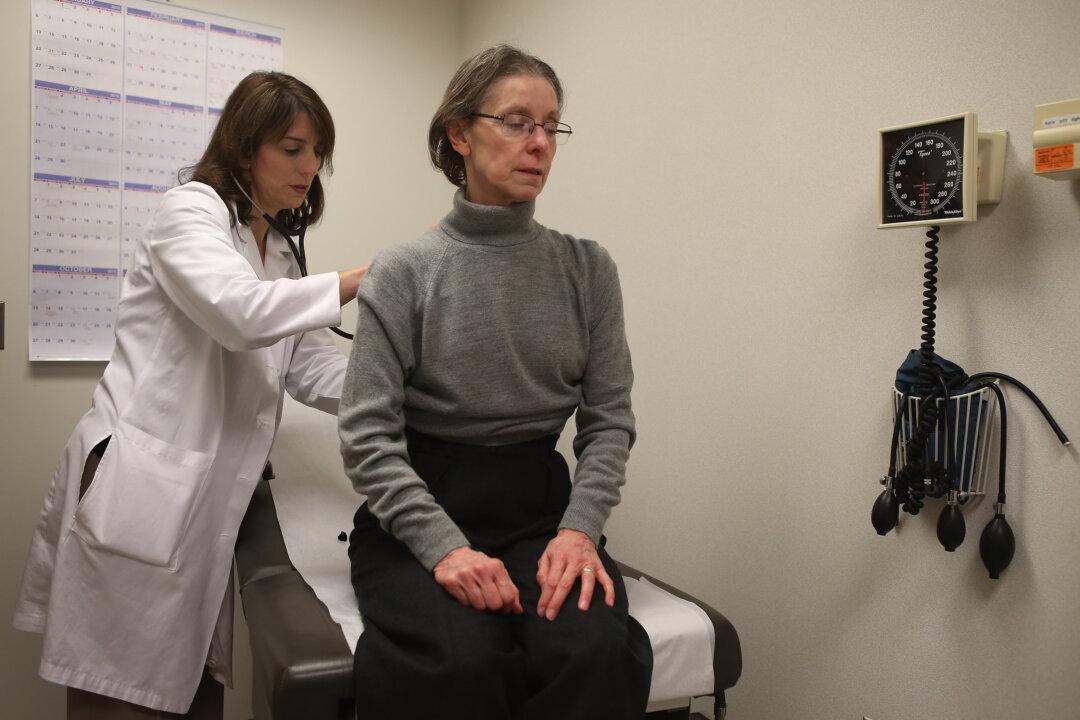
An increasing number of physicians across the United States are feeling burned out, so much so that it’s been deemed a “public health crisis,” a new report from Massachusetts health care organizations and Harvard institutes detailed.
The report, published Jan. 17, labels itself “a call to action” in turning the tide against the spreading phenomenon. The report’s authors say complicated computer interfaces and a growing burden of administrative tasks have pushed out physician engagement with patients and exacerbated the problem.