On his farm in Iowa, Matt Peters worked from dawn to dusk planting his 1,500 acres of fields with pesticide-treated seeds. “Every spring I worried about him,” said his wife, Ginnie. “Every spring I was glad when we were done.”
A clinical psychologist spoke to him on the phone and urged him to get medical help. “He said he had work to do, and I told him if it’s too wet in the morning to plant beans come see me,” Mike Rossman said. “And the next day I got the call.”In the spring of 2011, Ginnie Peters’ “calm, rational, loving” husband suddenly became depressed and agitated. “He told me ‘I feel paralyzed’,” she said. “He couldn’t sleep or think. Out of nowhere he was depressed.”
Peters took his own life. He was 55 years old.
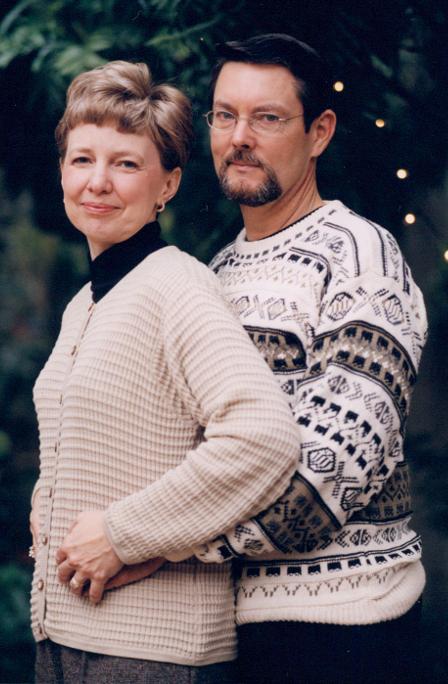
Matt Peters left behind his wife, Ginnie, and two children. Ginnie Peters




