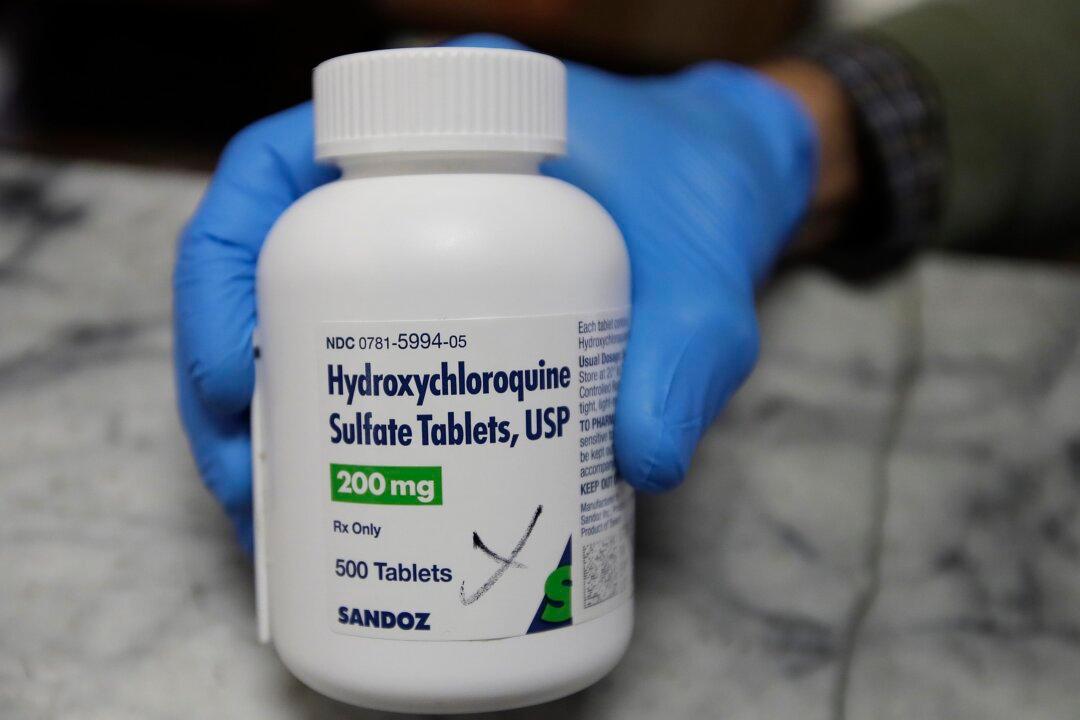
Doctors and experts on a panel created by the National Institutes of Health are recommending against using hydroxychloroquine, an anti-malaria drug, with azithromycin, an antibiotic known as Z-Pak, in the treatment of COVID-19.
The panel released its recommendations on Tuesday, including recommending against the combination, which is being used by a number of doctors in the United States and elsewhere.