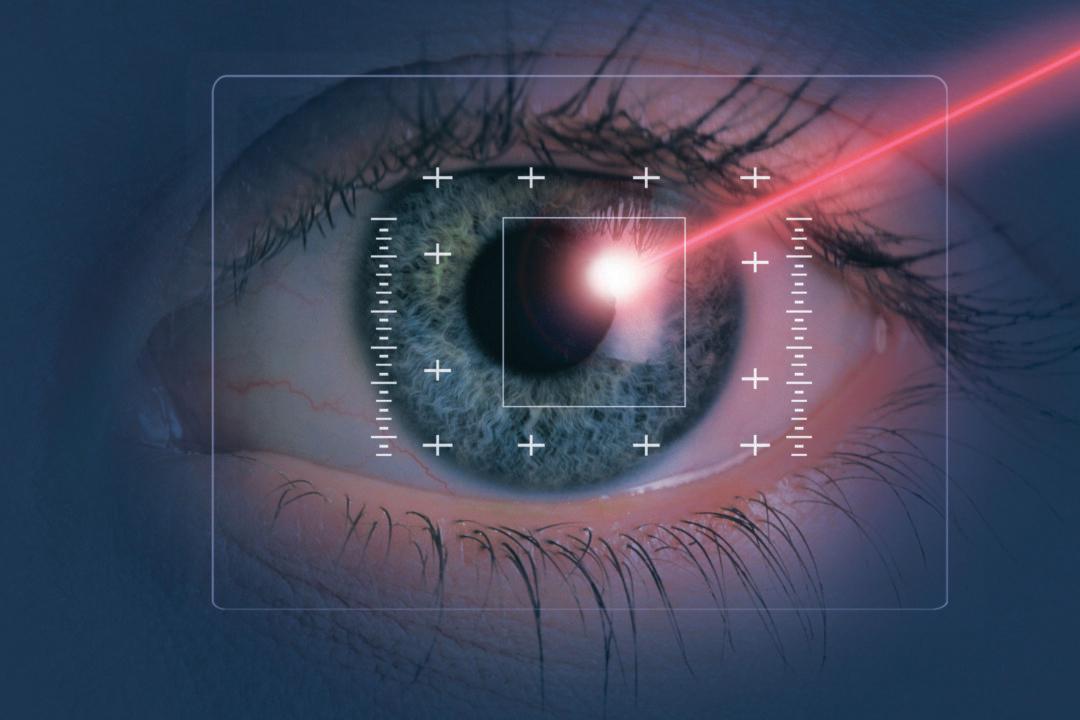
Myopia does not necessarily require a lifetime of wearing glasses. Nowadays, there is a way to restore normal vision–myopia laser surgery. However, in recent years, there has been a growing controversy regarding this type of surgery. Many studies and cases have shown that it may cause some people to lose their vision instead of gaining it, and it may even bring excruciating side effects.
After Paula Cofer underwent myopia laser surgery in 2000, her eyes became extremely dry and started to have a burning sensation. She has also been suffering severe nighttime vision loss, and was left with chronic pain. She has since posted many cases of severe complications from laser surgery on her website and Facebook page.