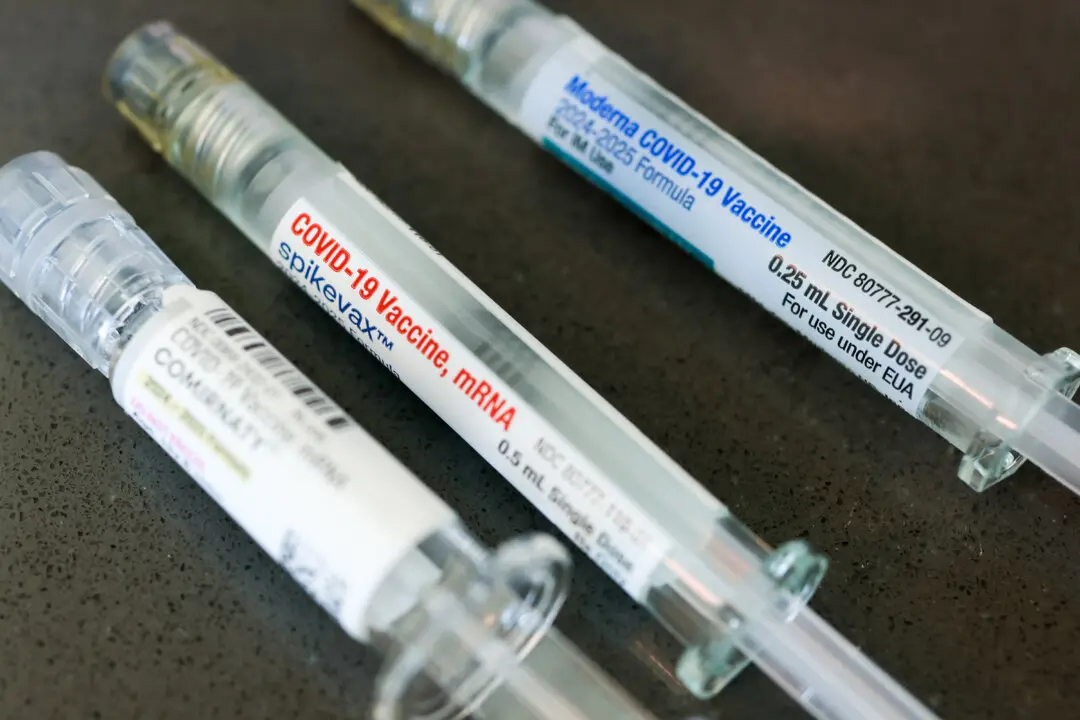
A CSIRO study has found MOFs (metal organic frameworks) to be a possible solution to address the challenge of transporting temperature-dependent vaccines.
According to the study, for vaccines to work with the maximum potency, they must be stored in specific conditions to avoid degradation across manufacturing, distribution, storage as well as administration; also known as the cold chain logistics.