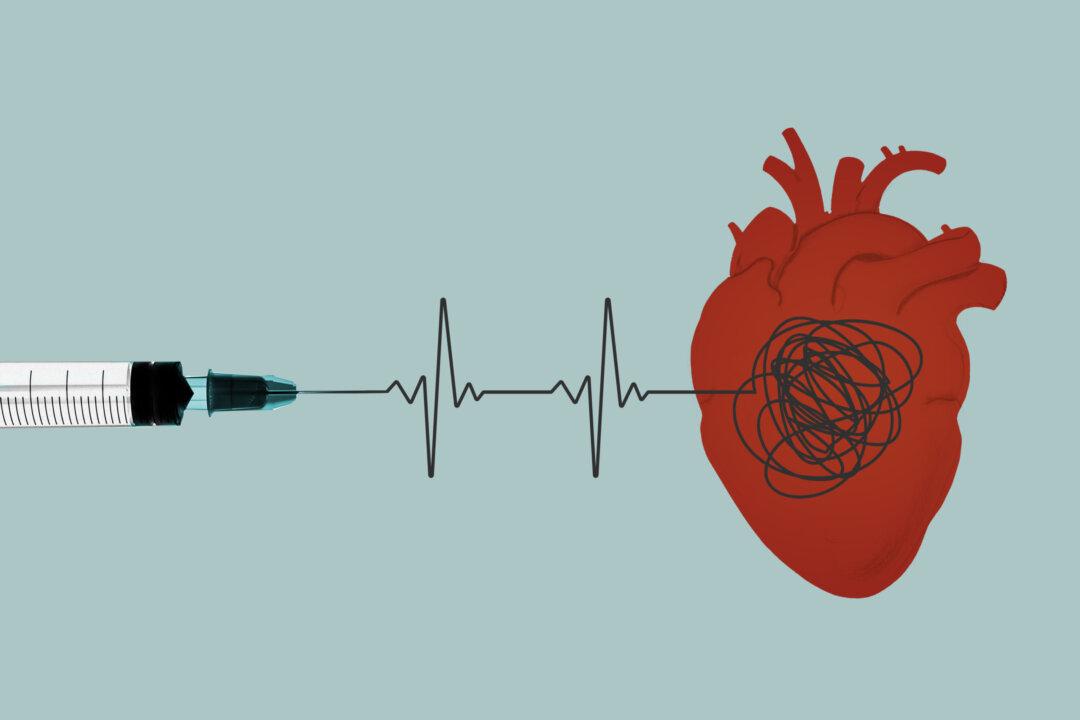
An Israeli Ministry of Health (MOH) study could not determine mortality risk from Pfizer’s COVID-19 vaccine and found no evidence of cardiovascular events after COVID-19 vaccination, the MOH said, though an outside expert said the conclusions are contrary to the data.
The study (pdf) was published in Hebrew on the MOH website on Feb. 27. The Epoch Times reviewed and translated the report.