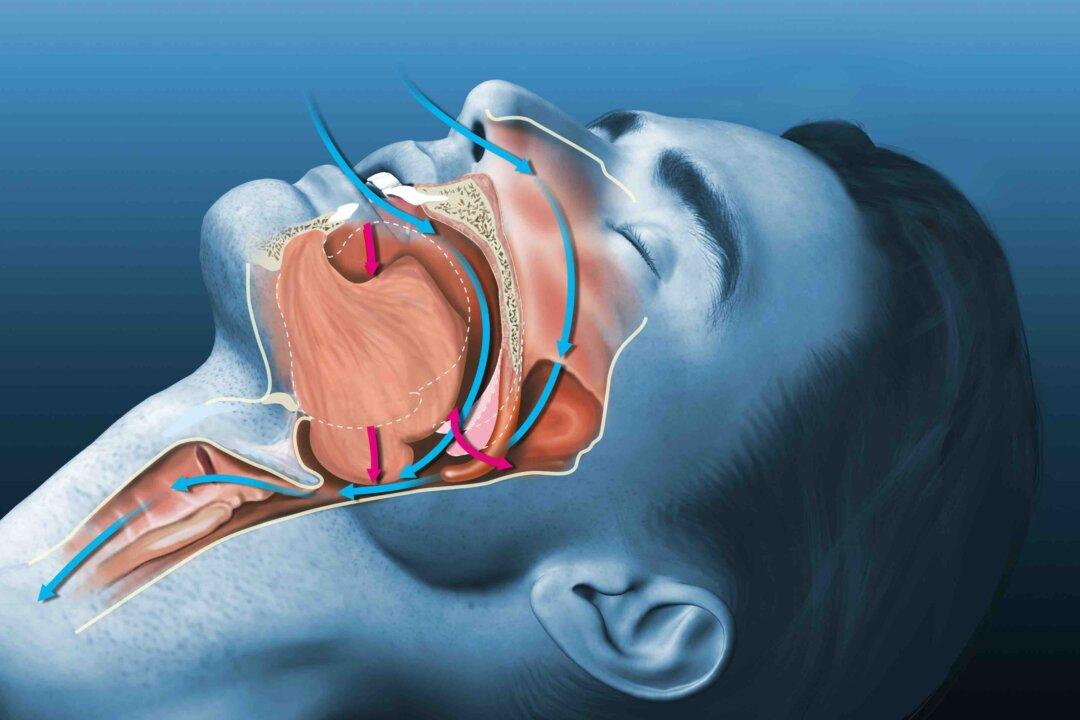
Apnea is a temporary cessation of breathing for at least 10 seconds.
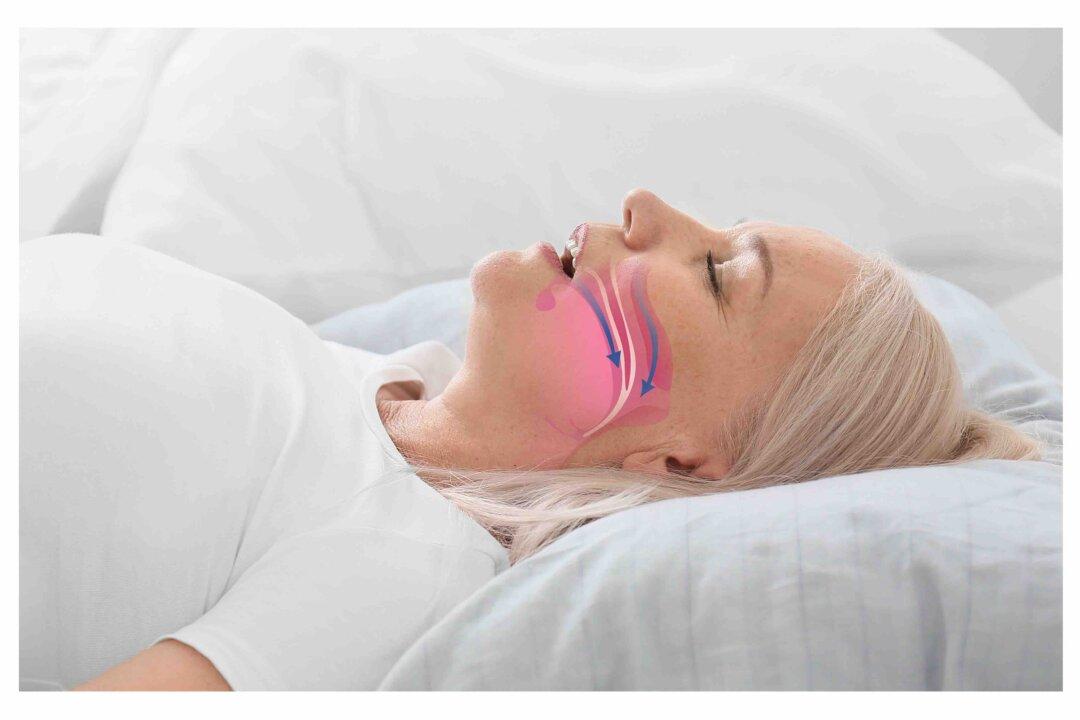
Obstructive sleep apnea (OSA) is the more common form of apnea that occurs when the throat muscles relax, causing the breathing to completely stop or reduce to 10 percent of the normal level.