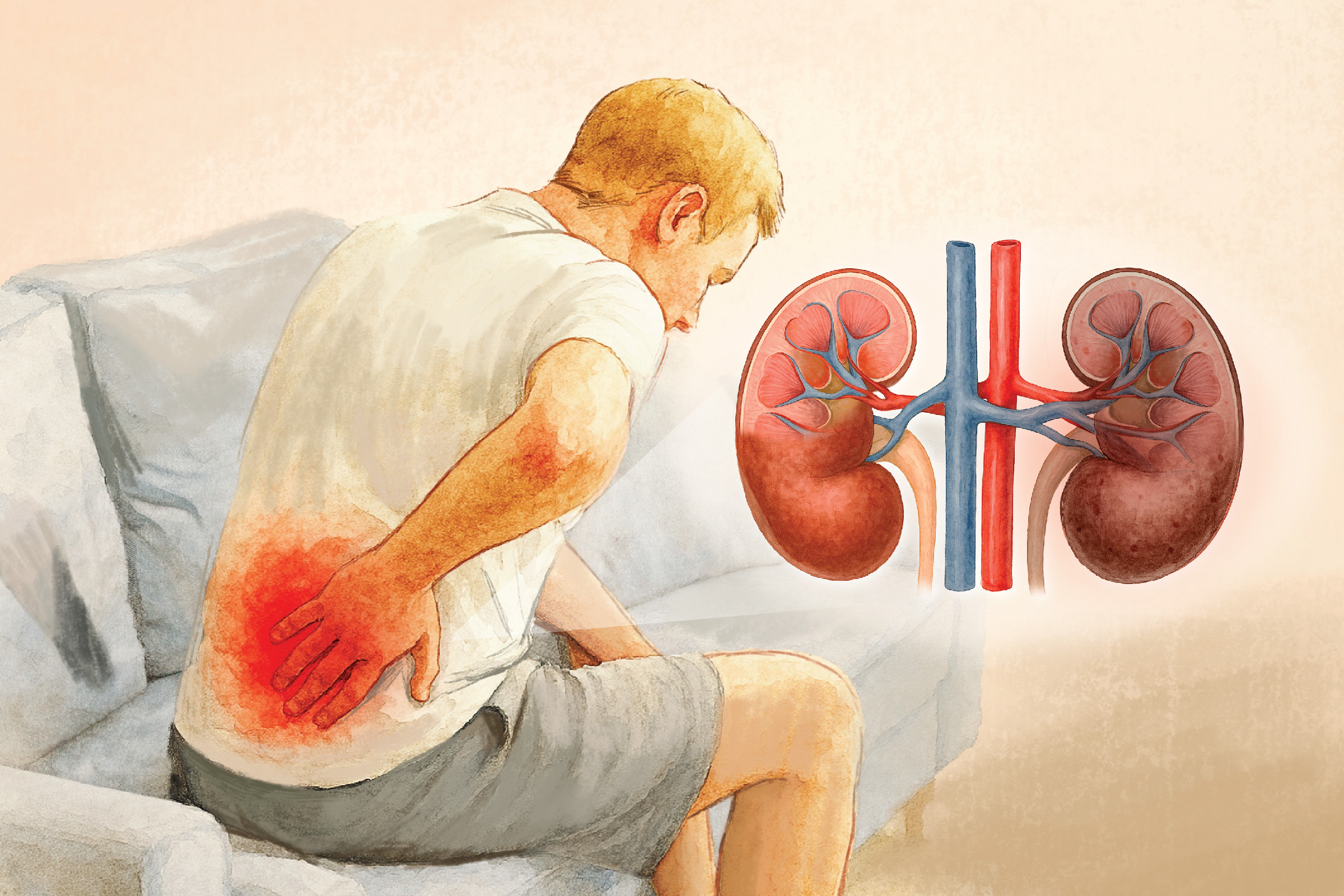
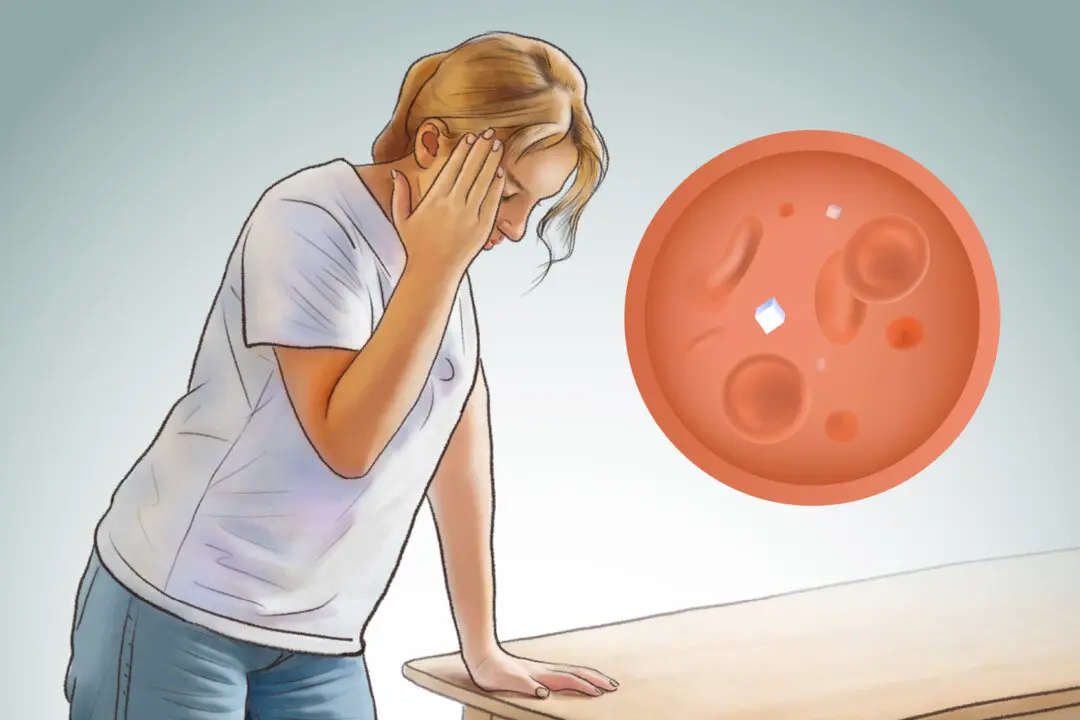
Literally meaning “urine in the blood,” uremia is a serious medical condition typically resulting from kidney failure, in which the kidneys can no longer filter out urea—a major organic component of urine—or metabolic waste products from the blood. Normally, these waste products are expelled through urine, but in uremia, they build up in the bloodstream. This leads to a toxic accumulation, causing a range of symptoms and complications beyond those of the underlying kidney disease.
Uremia, also called uremic syndrome, is caused by renal failure and is not a disease itself. The exact prevalence of uremia in the United States is difficult to determine because many end-stage kidney disease patients begin dialysis before developing uremic symptoms.