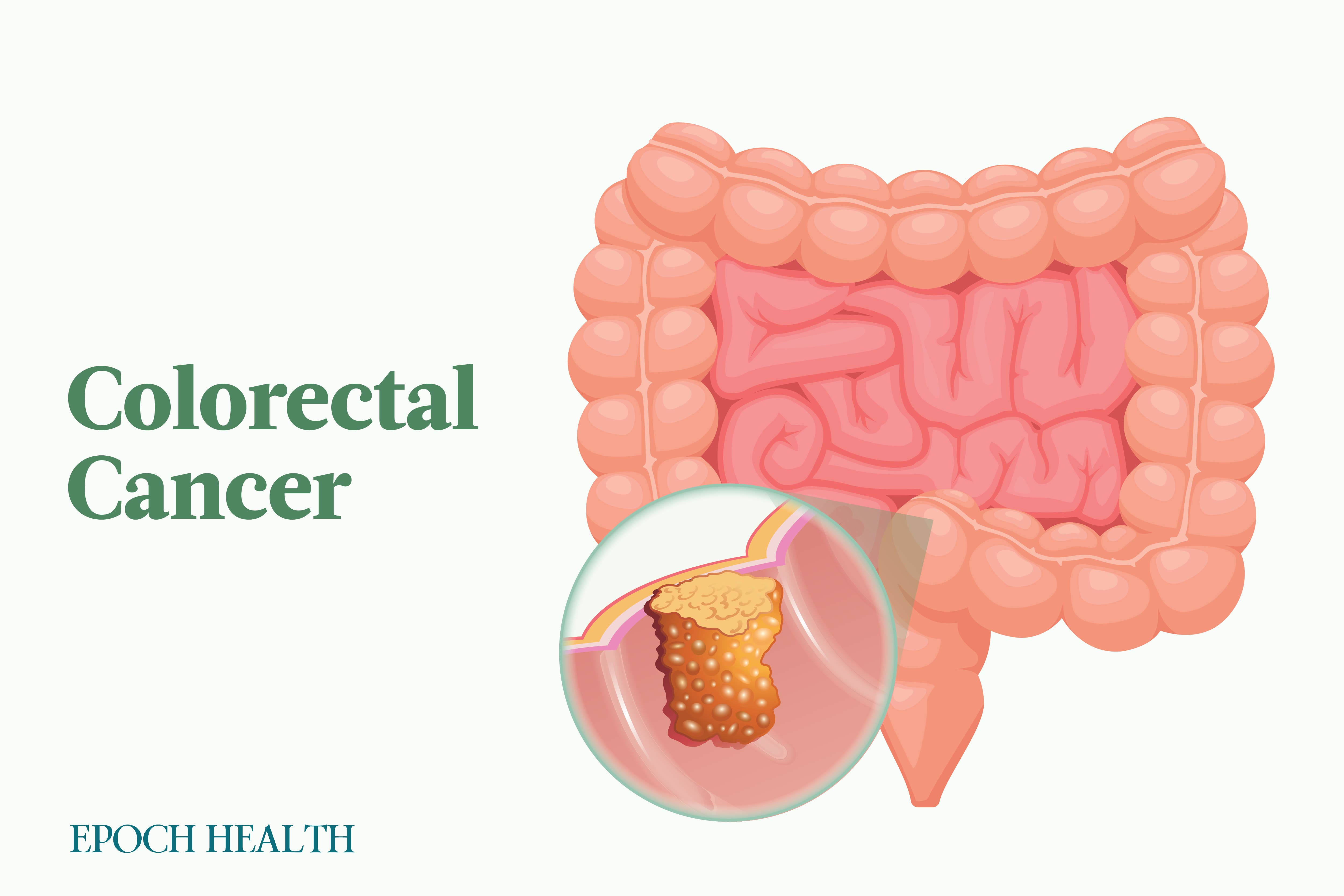
Colorectal cancer is the third most diagnosed cancer in both men and women in the United States. While overall incidence rates seem to be dropping, rates in people under 50 have increased by 1 to 2 percent yearly since the mid-1990s. In addition, colorectal cancer is responsible for the second leading cause of cancer-related deaths when fatality numbers for both men and women are combined.
Part of the challenge of diagnosing colorectal cancer is that it often does not present symptoms until it has spread. Once symptoms present, gastrointestinal (GI) tests are often completed to rule out other complications or causes.