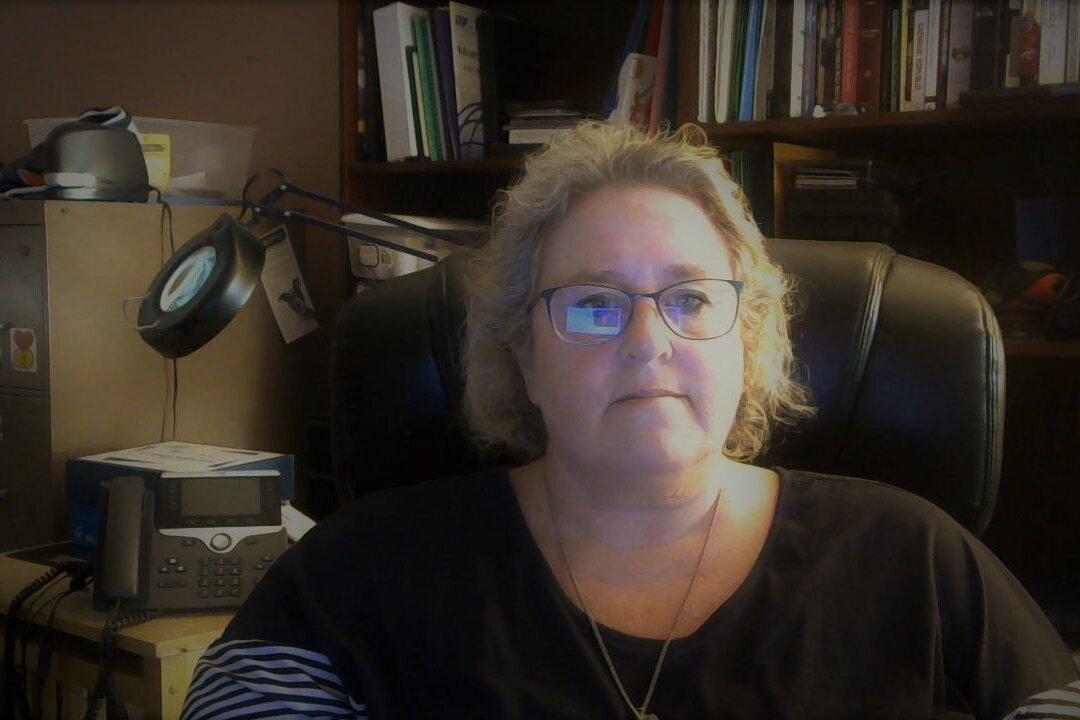
In an exclusive interview with The Defender, Gail Seiler describes how she was treated at a Texas hospital after they asked—and she told them—she wasn’t vaccinated.
This article was originally published by The Defender—Children’s Health Defense’s News & Views Website