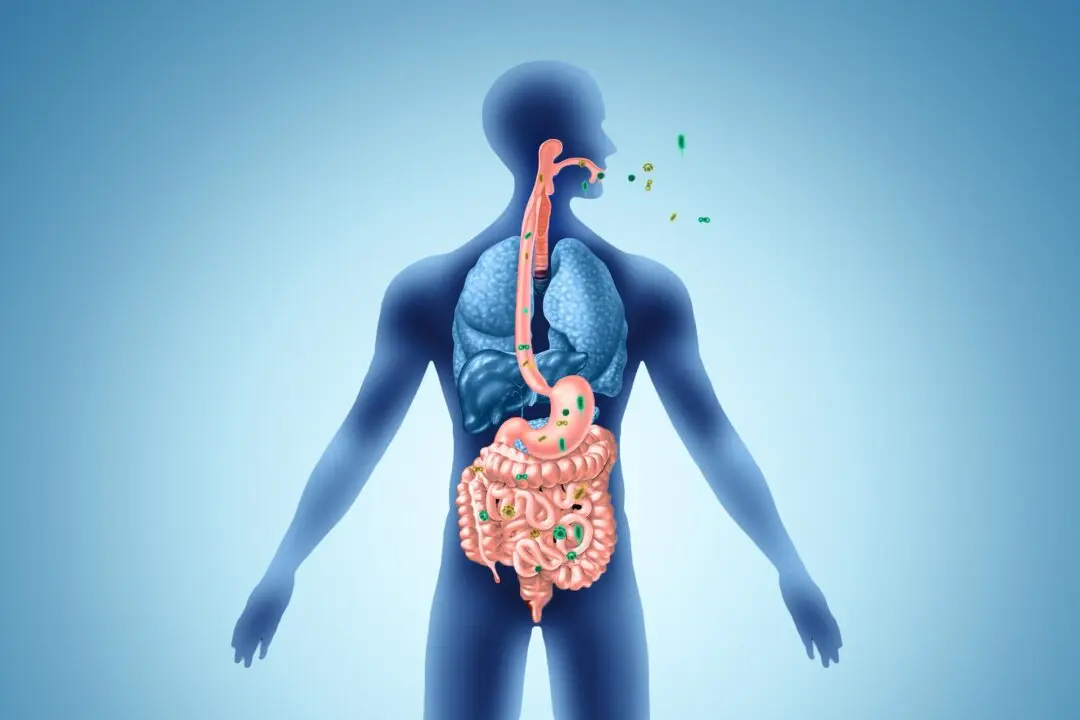
Microplastics in the environment may make bacteria harder to kill, a new study suggests.
The study, published in Applied and Environmental Microbiology by researchers from Boston University, found that bacteria exposed to microplastics develop resistance to multiple antibiotics commonly used to treat infections.