It’s time to move on.
The Alberta election is over: Danielle Smith is the premier and that means it is time for the politicians to put aside the campaign’s empty rhetoric and face the realities of how they can best fix a broken health-care system.
It is estimated that as many as 800,000 Albertans currently do not have a family doctor to guide their care. The province is leaking physicians and struggling to recruit doctors for family medicine positions, particularly in rural areas. It will take many years to ensure that each Albertan has a doctor to guide their care.
Nurses are being recruited (especially from abroad), but still far too many are leaving the profession due to poor working conditions and burnout.
Wait times for emergency responders, surgeries, and care at emergency departments were dire just one year ago but have improved somewhat since a government action plan was implemented in November 2022.
This plan made both a much-needed investment in human resources and innovative structural changes–hiring more paramedics and nurses, devising alternative methods (i.e., not ambulances) for transferring patients between facilities, farming out surgeries to non-hospital surgical centres, and creating room for acute care patients by transferring eligible patients to newly established continuing care spaces.
The government has said it is committed to continuing this action plan and given its relative success, Premier Smith should support the continued use of private providers in caring for patients. Almost every provincial government has turned to private clinics when surgery waitlists get too long; it’s time to stop pretending this doesn’t happen and give private providers an official role in health care delivery.
Another way Smith could improve and ensure the timely delivery of health care is to do away with a unique, yet antiquated, feature of our universal care system: the bulk funding of hospital services, also commonly known as global budgeting.
Currently, the government provides an annual sum of money to hospitals, and it is up to them to allocate funds to physicians’ services, procedures, and surgeries. If that budget runs out before year-end, the hospital has to stop doing certain types of surgeries, and wards are closed.
Under this budgeting system, each patient represents a cost to the system. It can’t be a customer-friendly system when treating fewer patients is the only way to stay within the budget!
A more appropriate alternative is activity-based funding whereby the money follows the patient through the system. Hospitals are paid for each procedure performed and for each patient treated. More patients and more surgeries mean more money for the hospital. Wards don’t close. Operating rooms aren’t shut down. Costs are often reduced and efficiencies improve. The government still pays for the patient’s care, but hospitals are incentivized to treat more patients.
A key obstacle to reform is, perhaps surprisingly, too much money. Alberta is the envy of the provinces in that its oil revenues have produced a $2.4 billion dollar budget surplus. More money is typically a positive but, in this case, too many financial resources could become an obstacle to making significant health-care reforms. It’s simply too easy to maintain the status quo by pouring more cash into a lower-performing system instead of making necessary or money-saving innovations.
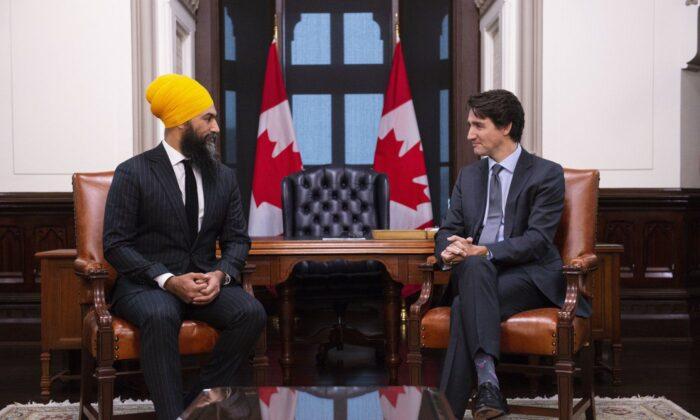
On a broader level, another obstacle to real health-care reform in Alberta is a stubborn and naïve reliance on universal health-care ideology. The NDP opposition party is ideologically (and, frankly, illogically) opposed to any structural reforms. It abides under the shibboleth that modern health care can be free, universal, and equally accessible to all Canadians.
That may have been true in the 1960s when the highest medical costs were physicians and hospital stays. But 60 years later, high-tech care that includes imaging, pharmaceuticals, and complicated surgeries has made it impossible for governments to provide enough money to take care of everyone and every health need. As a result, governments are forced to ration care, and patients are relegated to months- and years-long waitlists.
This increasingly stale, one-size-fits-all model also ensures as much health care as possible is delivered by the unionized public monopoly at a higher cost to taxpayers.
We may want to believe that we have universal medical care, but Canadians are increasingly forced to acknowledge the reality that our formerly beloved medical system is rapidly collapsing. Urgent attention is required and how Smith deals with it will undoubtedly be a key determiner of her success as premier.