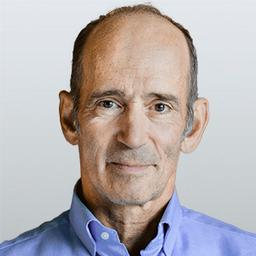
Florida’s new surgeon general, Dr. Joseph Ladapo, has issued a statewide public service announcement in support of commonsense COVID prevention strategies such as optimizing your vitamin D, staying active, eating nutrient-dense foods, and boosting your immune system with supplements.
Florida Health’s HealthierYouFL.org website now urges Floridians to “Talk to your health care provider about how certain supplements or foods containing vitamins and minerals might help boost your immune system, such as zinc, vitamin D, vitamin C and quercetin.” These are all well-known supplements that have been shown to have a positive impact on your COVID-19 risk.