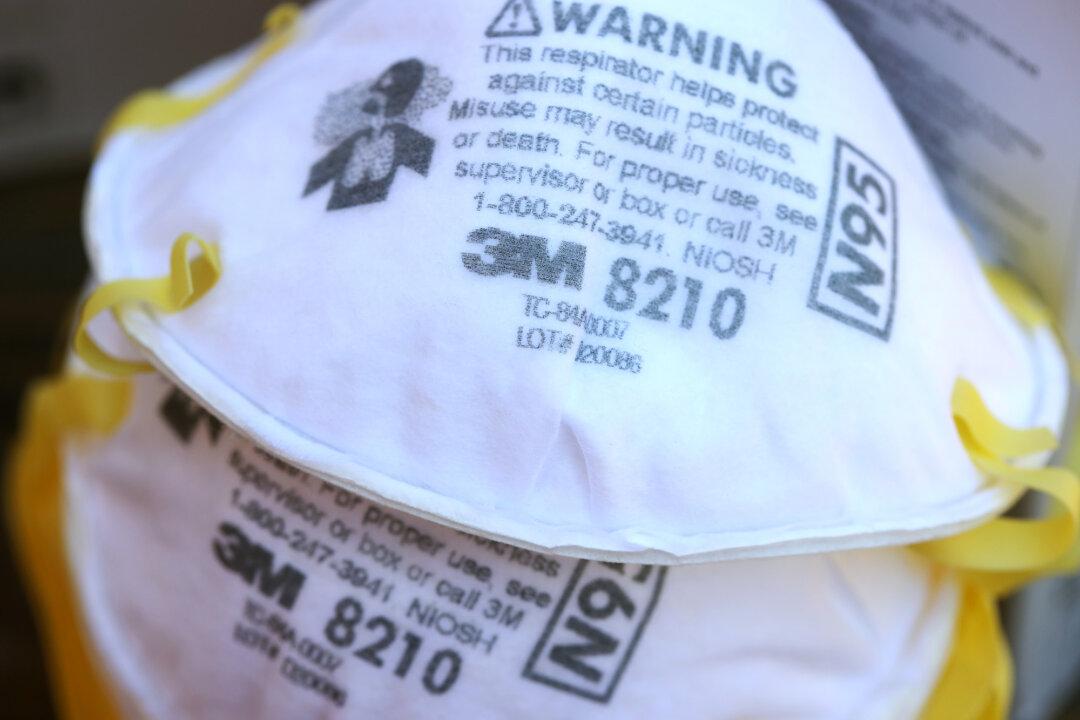
Entering a third year of the COVID-19 pandemic and the latest infection surge nationwide comes with many challenges. One of those is for a continued adequate supply of masks, including the often used N95 respirator masks for health care and other settings.
To combat any shortages of N95 masks during the pandemic, many institutions were forced to search for other alternatives to protect health care providers and their patients.