Critics of Democrats’ Inflation Reduction Act, as well as the Congressional Budget Office (CBO), are warning that the bill’s health care provisions could cause medical innovation in the United States, which leads the world in the sector, to decline sharply.
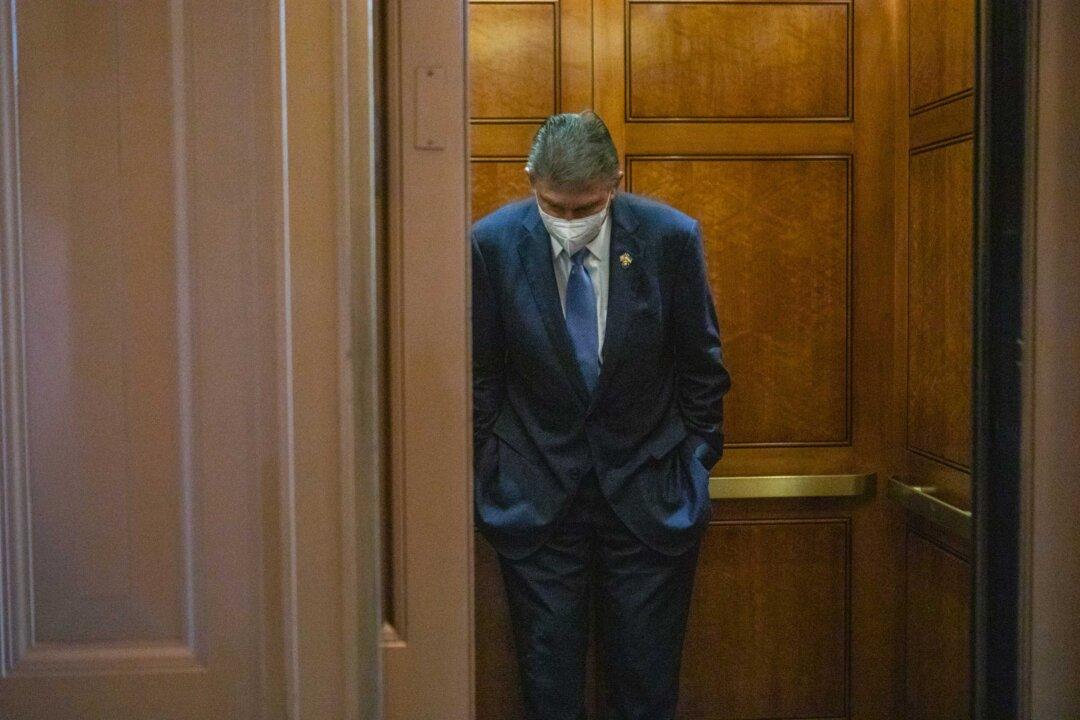
The measure, hammered out as a compromise agreement between moderate Sen. Joe Manchin (D-W.Va.) and Senate Majority Leader Chuck Schumer (D-N.Y.), serves to fulfill a series of broad Democratic aspirations: increasing federal revenue by closing so-called tax loopholes, enacting climate change policies, expanding the Affordable Care Act, and reducing prescription drug prices.