What is Autoimmunity?
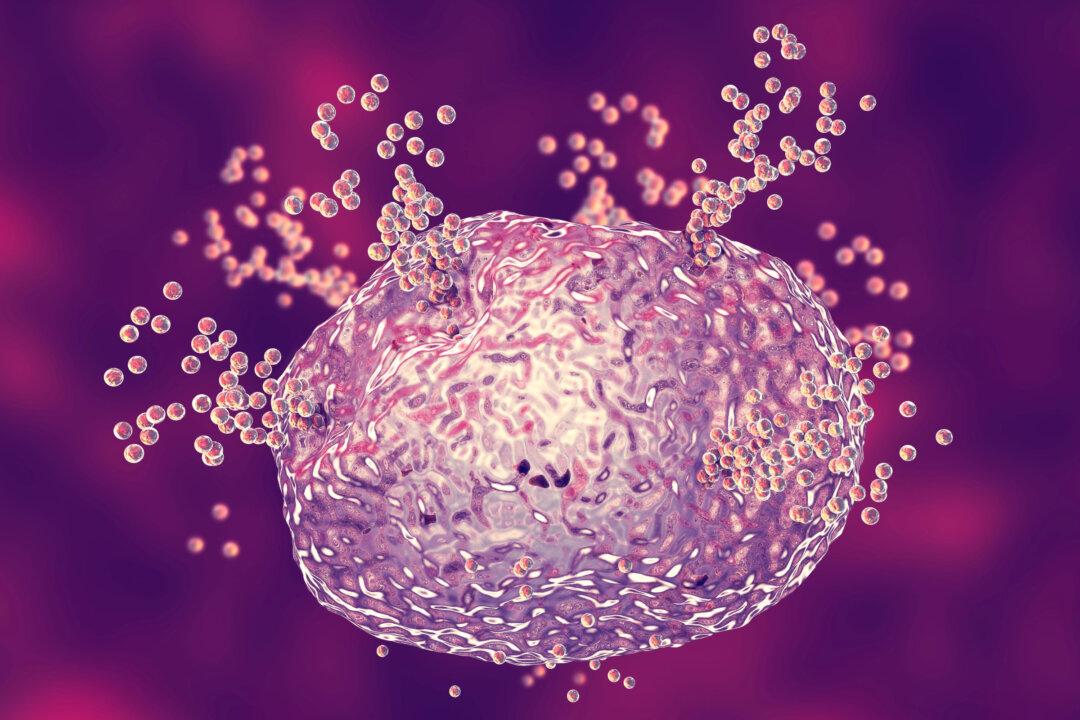
While the medical community at large does not recognize an exact root cause of autoimmune disease, the research is clear that many variables may contribute to autoimmune disease including genetic expression, internal and external environmental triggers, and hormonal changes. Seasons of stress and trauma have also been correlated with manifestations of autoimmune disease. All of these factors have the ability to disrupt the immune system and trigger autoimmune disease.To understand autoimmunity we need a foundational understanding of the immune system. The immune system is an intricate organization of various immune cells, organs, and biochemical messengers that work together to protect the body from foreign invaders. These foreign invaders include viruses, bacteria, parasites, environmental toxins, food, mold, and mycotoxins. When the body comes in contact with any of these threats, the immune system responds with an attack to overcome the threat. This is the body’s innate, natural defense mechanism often referred to as the inflammatory response.