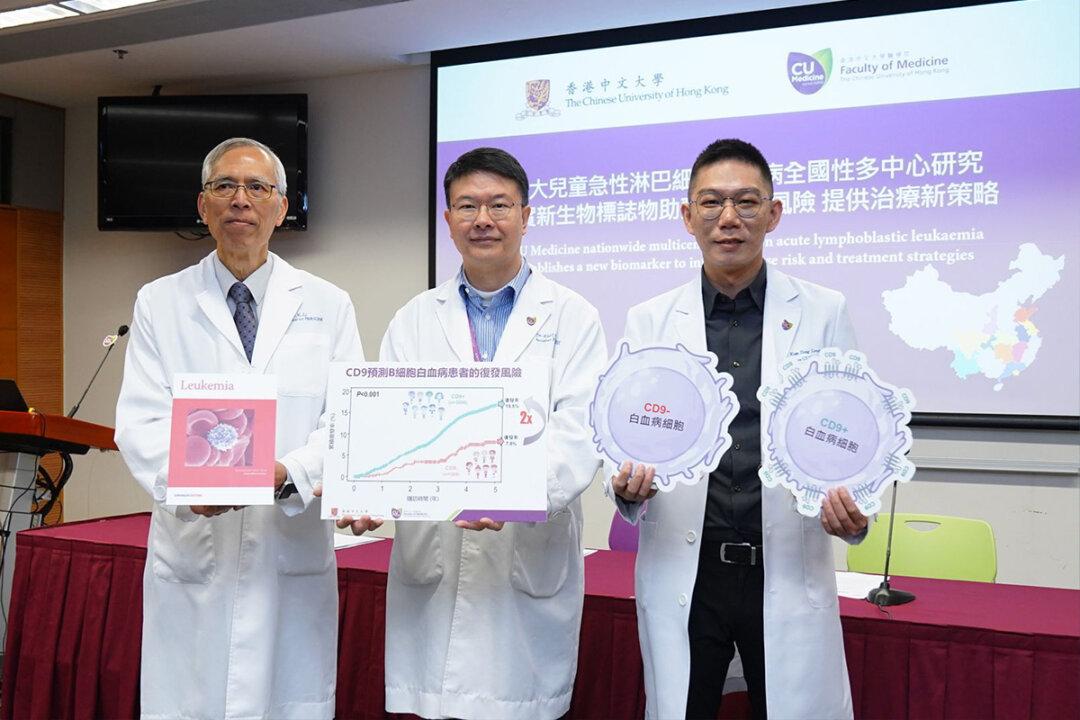
Acute lymphoblastic leukemia (ALL) is the most common children’s cancer. A study by the School of Medicine at CUHK confirmed that a protein called CD9 is closely related to the prognosis of children with ALL and can be used as an independent biomarker to predict the risk of recurrence, helping to identify high-risk patients and find appropriate treatment options as early as possible to reduce the risk of recurrence and improve survival rate.
According to CUHK, ALL accounts for about 30 percent of all children’s cancers, 90 percent of which are B-cell leukemia (B-ALL), and 10 percent are T-cell leukemia (T-ALL). Currently, there are about 50 new cases in Hong Kong every year.