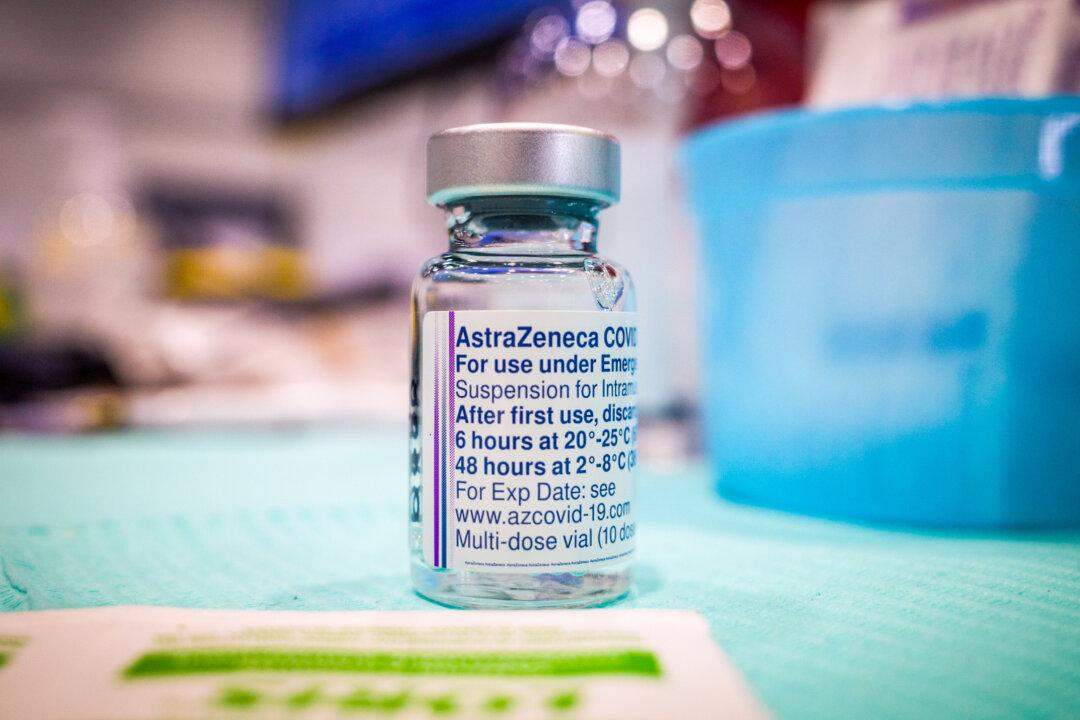
An American woman who suffered an injury from AstraZeneca’s COVID-19 vaccine sued the company on May 13, alleging the company breached a contract by not paying for the medical care she requires to deal with the injury.
“They left us no choice,” Brianne Dressen, a preschool teacher in Utah, told The Epoch Times in an email.