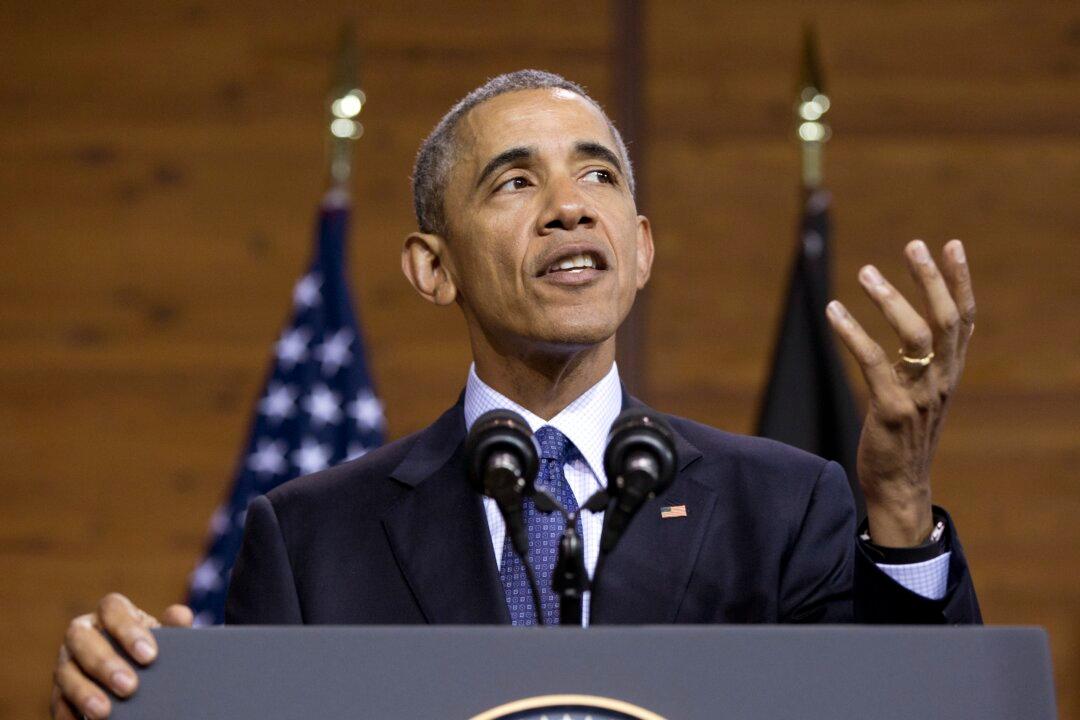
WASHINGTON—Expect insurers to seek significant premium increases under President Barack Obama’s health care law, in a wave of state-level requests rippling across the country ahead of the political conventions this summer.
Insurers say the law’s coverage has been a financial drain for many of them, and they’re setting the stage for 2017 hikes that in some cases could reach well into the double digits.
For example in Virginia, a state that reports early, nine insurers returning to the HealthCare.gov marketplace are seeking average premium increases that range from 9.4 percent to 37.1 percent. Those initial estimates filed with the state may change.
The health law’s insurance markets offer subsidized private plans, with more than 12 million customers enrolled nationwide. Going into their fourth year, they don’t yet seem to have achieved stability. That’s a contrast with more-established government programs like Medicaid and Medicare Advantage, in which private insurers profitably cover tens of millions of people.
The health law’s nagging problems seem to center on lower-than-hoped-for enrollment, sicker-than-expected customers, and a balky internal stabilization system that didn’t deliver as advertised and was already scheduled to be pared back next year.
This year, premiums for a benchmark silver plan rose by a little more than 7 percent on average, according to administration figures. Sharp increases for 2017 would fire up the long-running political debate over the divisive law, which persists despite two Supreme Court decisions upholding Obama’s signature program, and the president’s veto of a Republican repeal bill.