How much is a life worth?
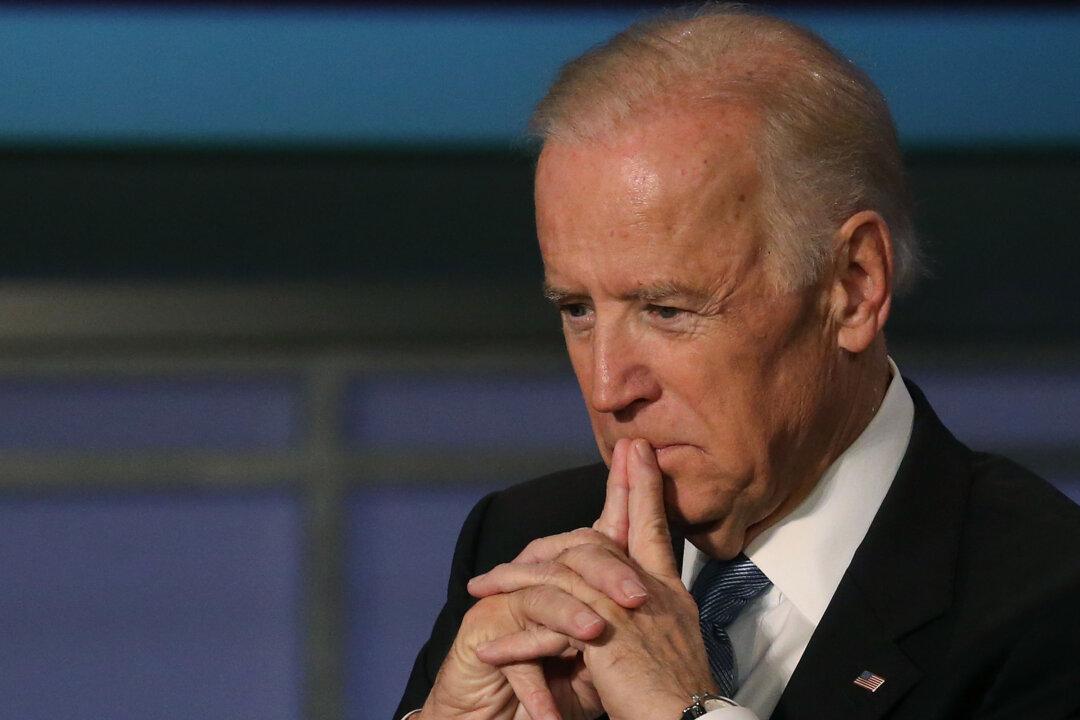
According to Vice President Biden, who lost his son Beau to brain cancer, quite a lot. In telling the country he wouldn’t run for president, Mr. Biden pledged to push for a moonshot program to cure cancer because, he said, there’s nothing more important.
Unfortunately, a small group of doctors is trying to undermine such efforts. In JAMA Oncology, some oncologists are encouraging health insurers to adopt “value-based” pricing, in which drugs are priced based on how long they extend the average patient’s life. The physicians say an experimental, advanced-stage lung-cancer drug isn’t worth more than $7,800 because it extends average life expectancy by “only” 1.6 months.
Under the value-based approach, insurers would impose their priorities on their patients, instead of letting them choose.