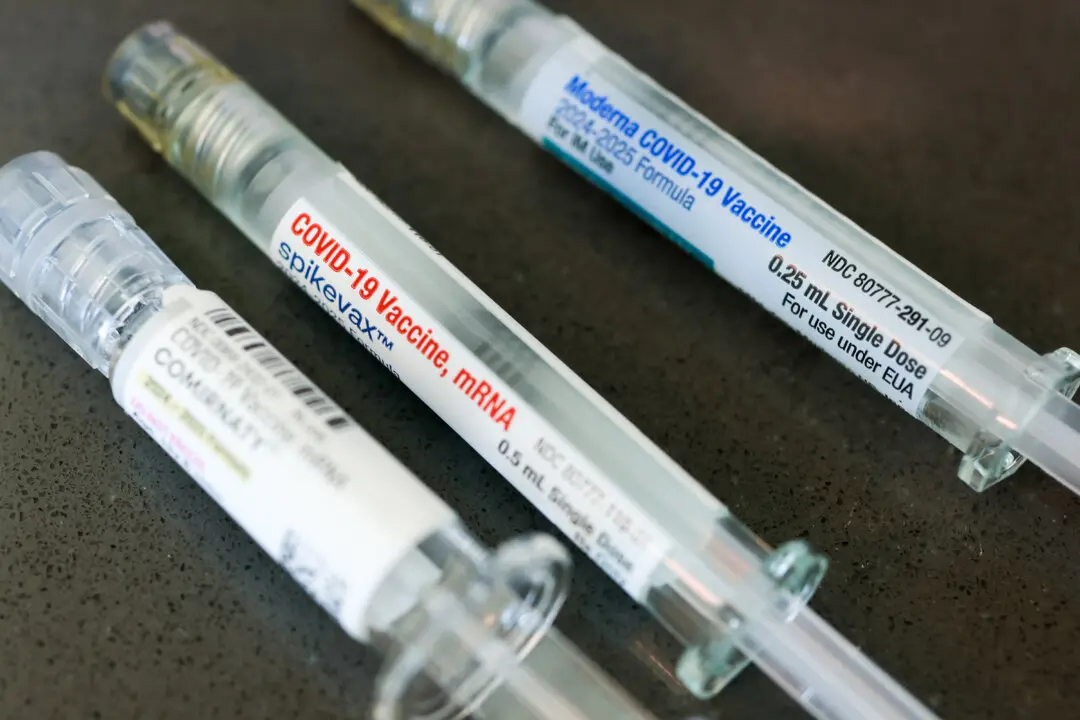
Moderna and regulatory agencies did not present clinical data on bivalent shots at the U.S. Food and Drug Administration (FDA) and the Centers for Disease Control and Prevention (CDC) committee meetings in June and September 2022, respectively.
Presentations to the FDA and CDC advisory committee excluded data from Moderna’s own clinical study that showed bivalent boosters may be no better at preventing infections than previous booster shots.