Ivermectin is a key drug for early COVID-19 treatment, Dr. Paul Marik says.
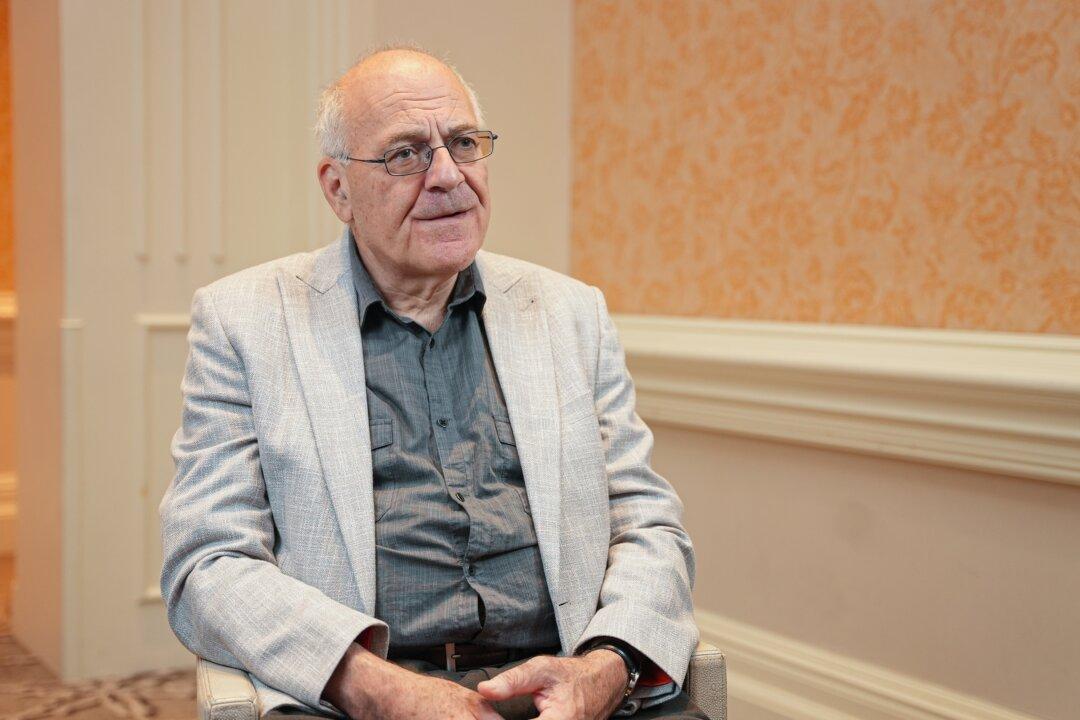
Dr. Paul Marik, co-founder of the Front Line COVID-19 Critical Care Alliance (FLCCC) and former Chief of the Division of Pulmonary and Critical Care Medicine at Eastern Virginia Medical School, at the FLCCC conference "Understanding & Treating Spike Protein-Induced Diseases" in Kissimmee, Fla. on Oct. 14, 2022. The Epoch Times
Zachary Stieber is a senior reporter for The Epoch Times based in Maryland. He covers U.S. and world news. Contact Zachary at [email protected]
Author’s Selected Articles