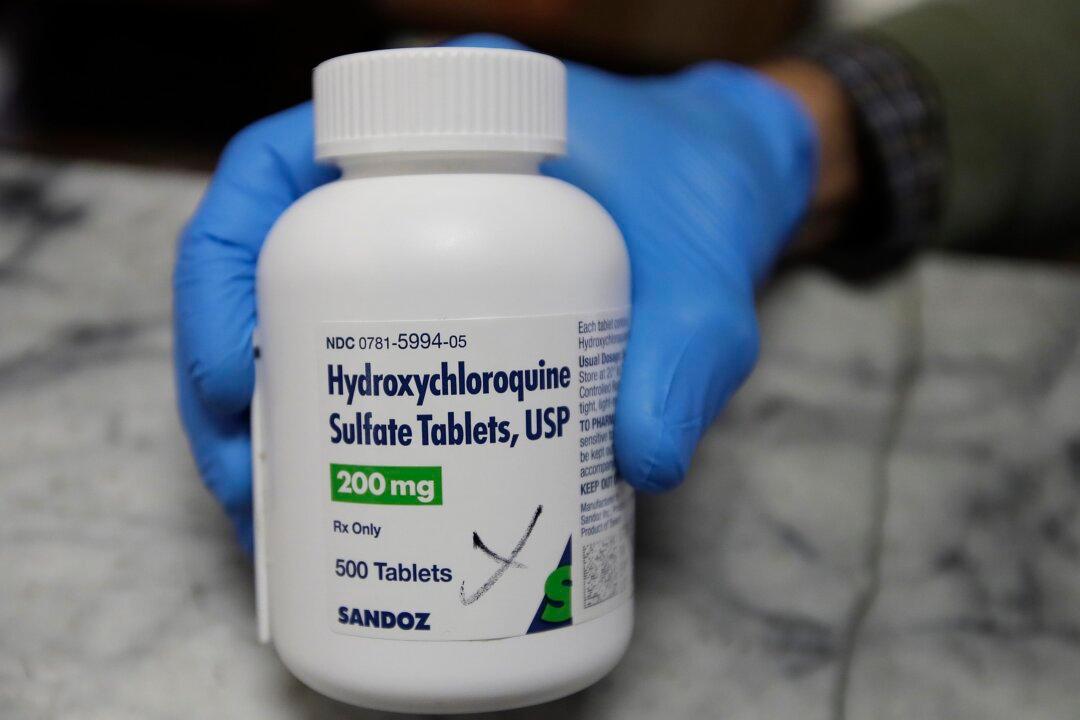
In a guideline published in the British Medical Journal on March 2, the World Health Organization (WHO) is advising against the use of hydroxychloroquine to prevent infection from the CCP virus, which causes the disease COVID-19.
The WHO assembled an international panel of experts—consisting of physicians, scientists, an ethicist, and four patients who recovered from COVID—to review data of six randomized controlled studies involving 6,059 participants who were or were not exposed to an individual with the CCP (Chinese Communist Party) virus.