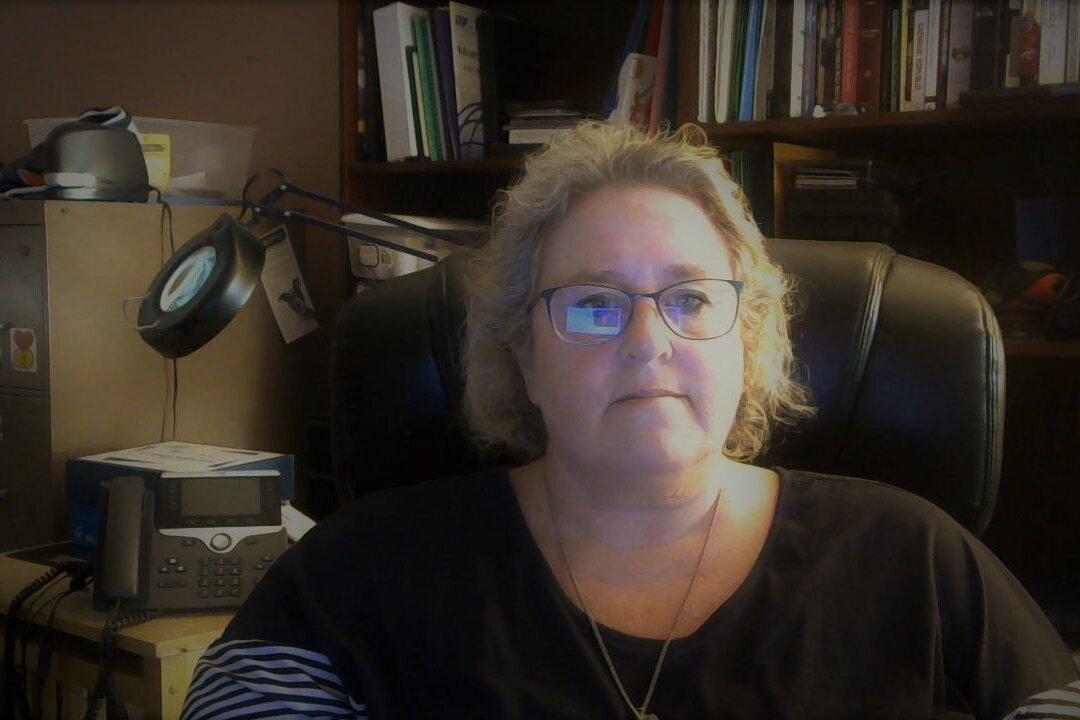
Over a week after Gail Seiler’s physician had given her a terminal diagnosis, her husband, Brad Seiler, wheeled her out of the back door of the hospital where she had been admitted for COVID-19 on Dec. 3, 2021.
“I’m so sorry, Mrs. Seiler, but you are going to die,” she recalled her physician telling her on Dec. 5.