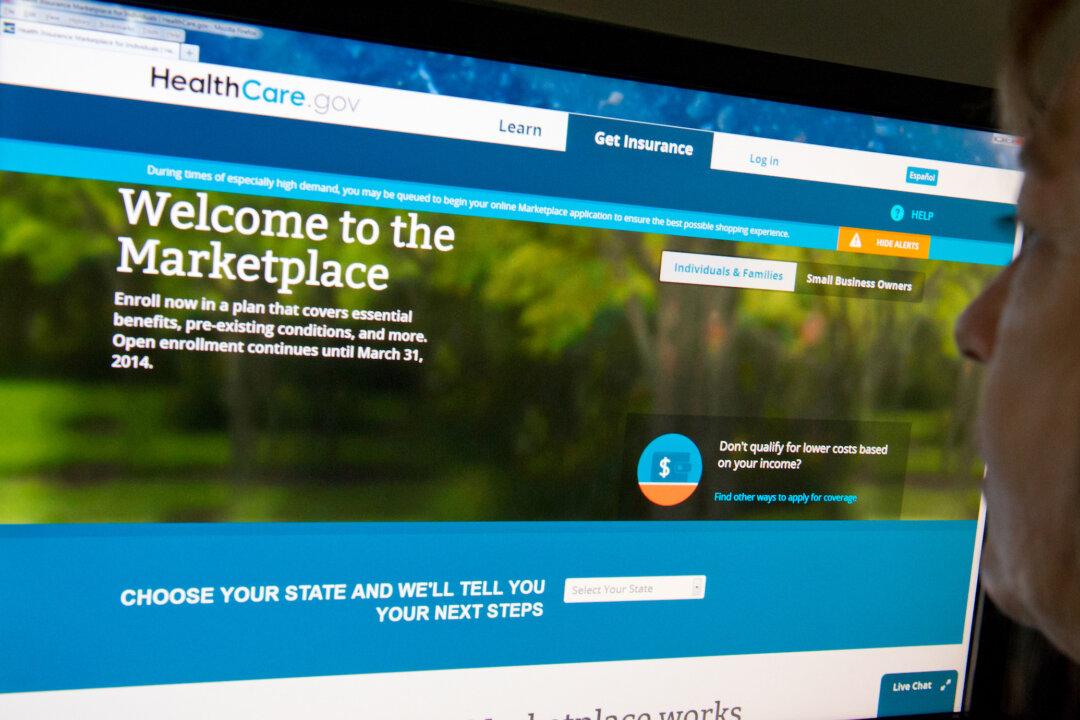
The Centers for Medicare & Medicaid Services (CMS) is advising states on how to provide more affordable health care options for people who don’t qualify for government aid.
The advice deals with a lack of federal funding for silver-level plans sold on the exchanges that likely has contributed to an increase in premiums for all plans.