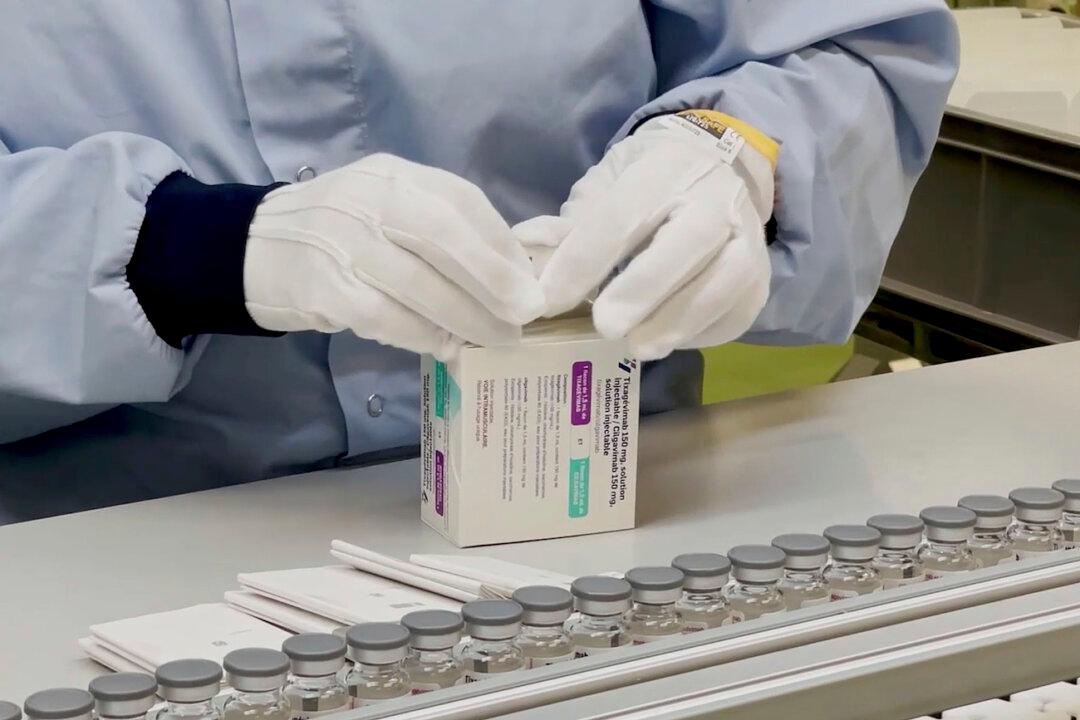
The U.S. Food and Drug Administration (FDA) issued an emergency use authorization on Dec. 8 for an AstraZeneca COVID-19 antibody drug designed to help prevent infection in people with compromised immune systems.
The drug, Evusheld, is a combination of two long-acting synthetic antibodies: tixagevimab and cilgavimab, which are derived from B-cells donated by patients who have recovered from the SARS-CoV-2 virus. It’s the first antibody therapy authorized in the United States for preventative COVID-19 treatment.