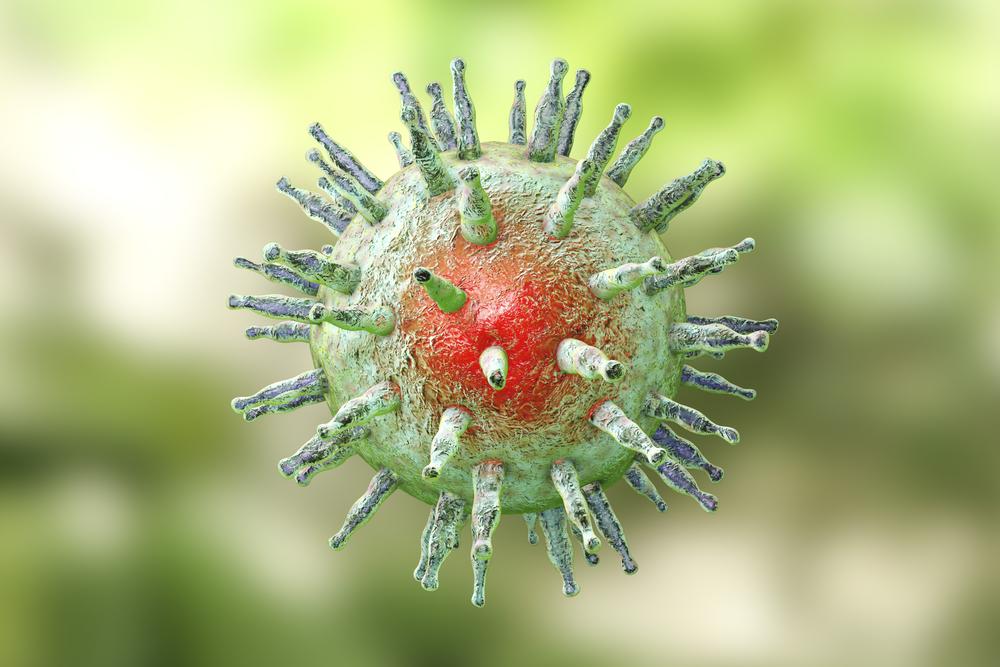
The Epstein-Barr virus (EBV) was confirmed as a major culprit of multiple sclerosis (MS) by scientists. EBV is actually ubiquitous in the population and infects up to 95 percent of adults.
For years, this was a suspected possibility.The suspicion has been confirmed by a Harvard study published in the journal Science in January 2022.